New research takes time to trickle into general knowledge. Old remedies and ways of thinking are bound to perpetuate for a while. However, in the case of blisters, the research is far from new. As you’ll see in the blister research timeline below, great blister research started in 1955 which tells us exactly what causes blisters and how to prevent them. So, why is the common understanding of what causes friction blisters of the feet still heat, moisture and friction? Why is it taking so long for our understanding of blister causation to become common knowledge?
The answer is not so much a problem of time, but one of translation. Research findings on the cause of blisters have not been successfully translated into a paradigm that make intuitive sense to the average person.
What Does The Blister Research Tell Us?
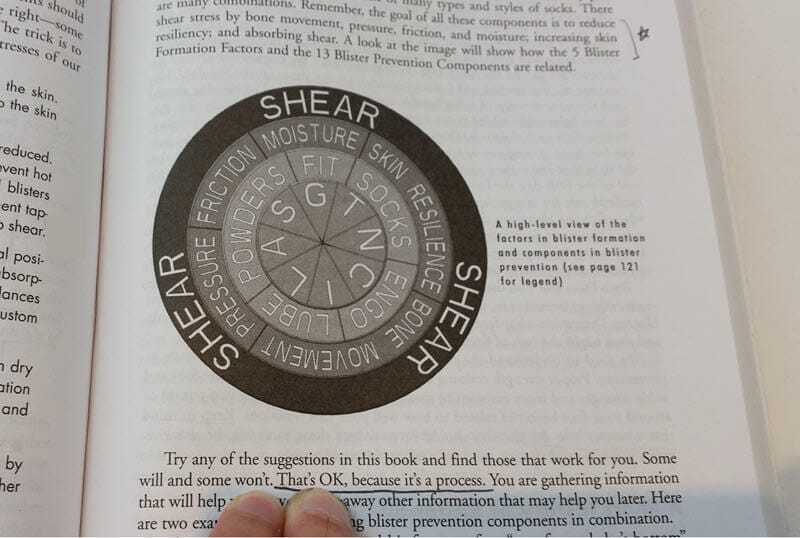
There is no doubt that friction blisters of the feet are caused by repetitive shear distortions. But don’t take my word for it. Here is a timeline of the best research and academic commentary on matters of blister causation. Specifically:
- Friction blisters of the feet are not a superficial-to-deep wear (rubbing) injury, they are a tear within the epidermis ie: under the sin surface.
- They’re also not a burn.
- Shear distortions are the mechanism of injury for friction blisters.
Here we go…
1955 – 1999 Blister Research
1955 Naylor (British Journal of Dermatology):
Naylor published two papers in 1955, both groundbreaking pieces of research. In July, he experimented with moisture’s effect on the coefficient of friction (COF). Friction was lower when dry, greasy or very wet, and increased when moist.
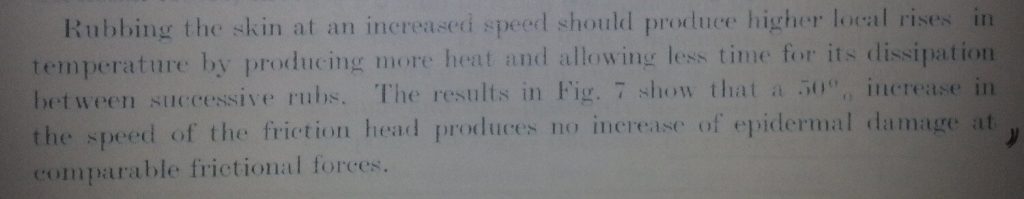
After that, in October, he produced blisters on 19 British medical students and doctors. Biopsies of these blisters showed that the tear occurred in the prickle layer of the epidermis (stratum spinosum) on every occasion. Significantly, by varying the thermal conductivity of the apparatus used (silver and polythene) and the speed of application, no change in rate of blister formation was found. It was this result that first suggested that a rise in skin temperature was unlikely to be responsible for blister formation.
Although not directly mentioned by Naylor, others have identified from his published data that friction levels were the main factor in determining how quickly the skin was damaged.
Further analysis and comment on Naylors work
a) “Some of Naylor’s data indicate that a relatively modest 30% reduction in COF would approximately triple the number of load cycles the skin could withstand before sustaining abrasive trauma. He demonstrated that vastly different rates of skin damage are possible with no change in the normal (compressive) component of the rub load. This finding, in 1955, still has not received due vigorous attention from most orthotic-prosthetic researchers and educators.” Carlson, 2006.
b) “On closer inspection of Naylor’s data, it is plausible to suggest that a reduction in CoF of approximately 30 % could increase the number of load cycles required to cause skin trauma by threefold. He therefore demonstrated that by keeping the compressive forces constant and manipulating only the friction loads, skin damage could still occur.” Hashmi, 2015.
c) “His data reveals that when friction loads were doubled, damage proceeded three times as fast (equal damage in one-third of the number of shear cycles). This was observed with no changes in the vertical/pressure component of the loadings”, Carlson, 2013.
- Naylor PFD. The skin surface and friction. BrJ Dermatol. 1955;67(7):239-248.
- Naylor PFD. Experimental friction blisters. Br J Dermatol. 1955;67(10):327-342.
1966 Sulzberger et al (Journal of Investigative Dermatology):
As an extension of Naylor’s blister research in 1955, Sulzberger’s team confirmed Naylor’s work by producing blisters on 54 American army personnel. It was confirmed that moisture increases skin friction, whereas very wet and very dry skin exhibited lower skin friction. Biopsies showed blisters to be a tear within the epidermis rather than a thermal burn.
They detailed the type of skin that most readily forms and maintains a blister. Their description of the ‘to-and-fro’ of shearing is poignant: The first is a sufficiently firm attachment of the lower epidermis to the underlying tissue. This enables the frictional forces at the surface to be transmitted through the superficial layers of the epidermis (stratum corneum and granulosum) which are moved to-and-fro over the subadjacent layers, and thus by shearing, create a zone of damage or cleavage. The second prerequisite is a sufficiently thick or resistant stratum corneum and granulosum to withstand the degrees of surface friction required to produce the deeper damage which causes blistering.”
- Sulzberger MB, Córtese TA, Fishman L, Wiley FIS. Studies on blisters produced by friction I – Results of linear rubbing and twisting technics. J Invest Dermatol. 1966;47(5):456-465.
1968 Spence and Shields (Journal Of The American Podiatric Medical Association):
Blisters are not the only manifestation of repetitive shear distortion, as mentioned by these researchers. “Blisters, callosities and ulcers are primarily caused by excessive shear forces, commonly referred to as friction, acting on the skin.” Note that they allude to the lack of clarity about the definition of shear forces and friction.
- Spence WR, Shields MN. Prevention of blisters, callosities and ulcers by absorption of shear forces. J Am Podiatr Med Assoc. 1968;58(10):428-434.
1969 Griffin et al (The Journal Of Investigative Dermatology):
Another experimental blister study, this one concluded that while blisters form faster in warm temperatures compared to cold, the skin temperature didn’t exceed 44 degrees Celsius, insufficient to cause a burn blister. Additionally, friction blisters and burn blisters are different histologically.
- Griffin CPT, Cortese TA, Layton LL, Sulzberger MB. Inverse time and temperature relationship in experimental friction blisters. J Invest Dermatol. 1969;52(Morning Session):384-401.
1972 Akers & Sulzberger (Military Medicine):
Akers and Sulzberger produced experimental blisters to look deeper into the frictional forces required to create them. They reiterate that blisters are not a thermal burn but are in fact the result of shear causing a tear in the epidermis.
Most significantly, they described the concept of friction management in preventing blisters “…in order to promote slippage and prevent blisters.” Additionally, “Since friction blisters are not burns but are due to shearing forces in the epidermis, on purely theoretical grounds, foot-gear which takes up the differential movement, not in the epidermis but before it reaches the skin surface, would be likely to reduce blistering.”
- Akers WA, Sulzberger MB. The Friction Blister. Mil Med. 1972;137(l):l-7.
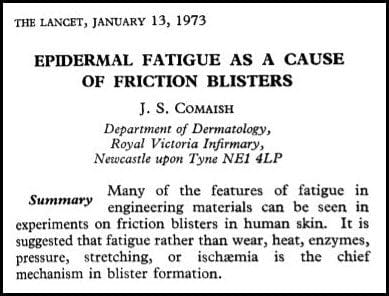
1973 Comaish (The Lancet):
Comaish applied the principals of engineering to determine the cause of blisters. He found that rather than wear, heat, enzymes, pressure, stretching or ischaemia, blisters are a “mechanical fatigue due to shearing force horizontal to the skin surface.”
- Comaish JS. Epidermal fatigue as a cause of friction blisters. Lancet. Published online 1973:81- 83.
1977 Akers (International Journal of Dermatology):
Akers reiterates his results from 1972. Significantly, rubbing increased temperatures by only 3.5 degrees Celsius (in 4 volunteers) which was insufficient to cause a burn. [It is worth mentioning that blisters from thermal burns are by definition, second degree burns.]
- William A Akers. Sulzberger on friction blistering. Int J Dermatology. 1977;16(June):369-372.
1983 Brand (The Star):
Famously, Paul Brand, a leader in shear-related skin damage is quoted as saying “There are two types of force which occur on the sole of the foot, one is vertical force at right angles to the foot, which causes direct pressure on the tissues. The other is horizontal force, or shear stress, which is parallel to the surface of the foot and occurs in association with acceleration and deceleration. Of the two forces shear stress is more damaging than pressure.”
While this quote is recognised as significant and undeniably important, it also muddies the water a little. It combines ‘horizontal force’, which we know as the force of friction, with ‘shear stress’ as having the same meaning.
- Brand P. Neuropathic ulceration. The Star – National Hansen’s Disease Center. May 1983.
1985 Akers (American Journal of Industrial Medicine):
This paper provides a brief overview of the literature to date that shows local temperature increases are not responsible for a thermal burn blister and reaffirms that blisters are of mechanical origin ie: shear injury.
Significantly, Akers discusses the concept of friction, more particularly, static and dynamic coefficients of friction. The difference between static and dynamic friction is very helpful in understanding the concept of friction, shear and blister formation.
- Akers WA. Measurements of Friction Injuries in Man. Am J Ind Med. 1985;8:473-481.
1990 & 1993 Herring and Richie (Journal Of The American Podiatric Medical Association):
Herring and Richie carried out a double-blind study in 1990 on sock fibres and blistering. Significantly, they followed it up with another in 1993. They concluded that thick socks prevented blisters irrespective of the fibres used. The researchers indicated this effect could have come via an increased moisture-wicking effect available when the sock is thicker. But it could additionally be due to the extra blister prevention mechanism of “shear absorption”. The thick nap of the sock absorbs shear distortions with every step, so the soft tissues of the foot shear less.
- Herring KM, Richie DH. Friction blisters and sock fiber composition. A double-blind study. J Am Podiatr Med Assoc. 1990;80(2):63-71.
- Herring KM and Richie DH. Comparison of cotton and acrylic socks using a generic cushion sole design for runners. J Am Podiatr Med Assoc. 1993;83(9):515-522.
1995 Knapik et al (Sports Medicine):
As a comprehensive review of the blister research literature to date, this peper is very readable and full of pearls. For instance, this excerpt is notable: “Skin temperature appears to be a minor factor in blister formation. Blisters form somewhat more rapidly when the skin temperature is higher but blisters also occur when the skin temperature is low. In experimental rubbing studies, local heat is produced and skin temperatures have been reported between 41 degrees Celsius and 50 degrees Celsius. However, friction blisters do not resemble second degree thermal burns either clinically or histologically.”
This is a must-read article – link here.
- Knapik JJ, Reynolds KL, Duplantis KL, Jones BH. Friction Blisters: Pathophysiology, Prevention and Treatment. Sport Med. Published online 1995. doi:10.2165/00007256-199520030-00002
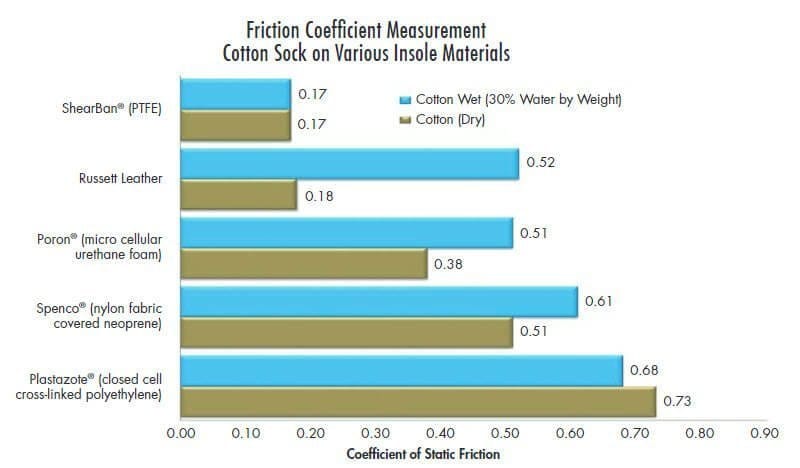
1998 Sanders et al (Journal of Rehabilitation Research and Development):
Sanders studied coefficient of friction (COF) data with and without wool socks against the following orthotics and prosthetics materials: Spenco, Poron, Medium Pelite, Firm Plastazote (LD70), Medium Plastazote (LD45), and Nickelplast.C. There was a trend of a higher COF at sock-material interfaces than at skin-sock interfaces.
- Sanders JE, Greve JM, Mitchell SB, Zachariah SG. Material properties of commonly-used interface materials and their static coefficients of friction with skin and socks. J Rehabil Res Dev. 1998;35(2):161-176.
1999 Zhang & Mak (Prosthetics and Orthotics International):
The coefficient of friction between the skin and five commonly-used materials were tested. These included cotton, nylon and silicone. Silicone was found to have the highest COF, followed by cotton. Nylon had the lowest COF. Within the introduction, the authors make this insightful comment:
“The injurious effects of friction on the skin and the underlying tissues can be divided into two classes, those without slip and those with slip. The former may rupture the epidermis and occlude blood and interstitial fluid flows by stretching or compressing the skin. The latter adds an abrasion to this damage.”
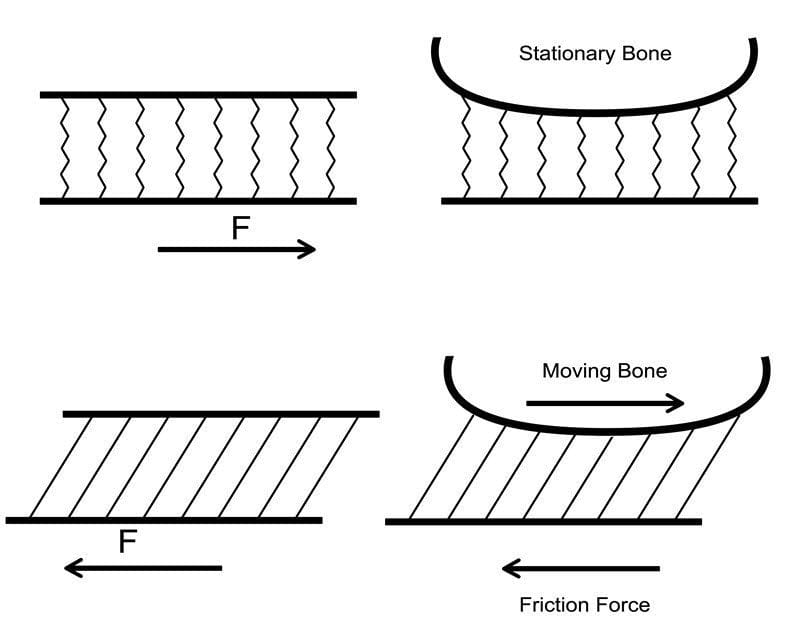
This describes strategic friction management. It can be difficult for the uninitiated to reconcile that the aim is to allow the foot to slip. However, we don’t want the whole foot to slip and slide within the shoe – just the blister susceptible area of skin. This is how we enable the skin to move in sync with the underlying bone, thus reducing the magnitude of shear distortion.
- Zhang M, Mak AFT. In vivo friction properties of human skin. Prosthet Orthot Int. 1999;23:135-141.
2000 – 2009 Blister Research
2000 Hosein & Lord (Clinical Biomechanics):
These researchers published two papers measuring shear on the sole of the foot while walking, first in “normal” subjects, then in a group of neuropathic diabetics. These were among the first studies to use apparatus to measure shear whilst walking. In this case, via transducers attached to an insole. In their introduction of their first paper, this comment: “Mechanical stress has two components, namely pressure and shear. Only pressure is widely reported. The plantar shear component has as yet had little investigation, mainly due to the lack of technology for its measurement.”
And this from the second paper: Mechanical stress at the plantar interface has two components, pressure acting normal to the surface and shear acting tangential to the surface. Shear has as yet had little investigation. This is mainly due to the paucity of suitable technology for its measurement until recently.”
- Hosein R, Lord M. A study of in-shoe plantar shear in normals. Clin Biomech. 2000;15:46-53.
- Lord M, Hosein R. A study of in-shoe plantar shear in patients with diabetic neuropathy. Clin Biomech. 2000;15:278-283.
2000 Curryer & Lemaire (Journal Of The American Podiatric Medical Association):
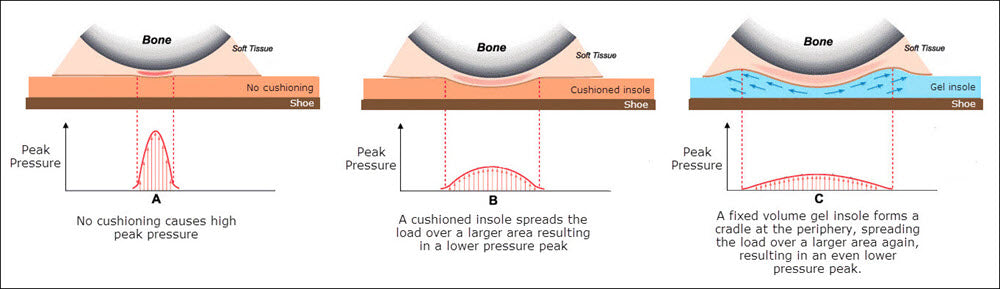
This time using materials taped to a floor-mounted force plate, five materials were compared for their effectiveness to reduce shear forces under the sole of the foot. The two gel materials, Silipos Soft Shear and Silipos Conformagel, were found to be more effective than foams Spenco, PPT and Plastazote.
This is an excerpt from their introduction: “During walking, the sole of the foot is subjected to mechanical stresses. These stresses comprise two components: direct pressure perpendicular to the surface (vertical) and shear forces tangential to the surface (horizontal).”
- Curryer M, Lemaire ED. Effectiveness of Various Materials in Reducing Plantar Shear Forces – A Pilot Study. J Am Podiatr Med Assoc. 2000;90(7).
2001 Carlson (OrthoKinetic Review):
Carlson discusses our focus on pressure instead of friction. “The long-ignored knowledge about repetitive-loading skin trauma was discovered and first published in the 1950s and 1960s. Straightforward experiments by P.F.D. Naylor in the early 1950’s demonstrated that the perpendicular load component by itself is relatively harmless. Those experiments established that the magnitude of repeated pressure peaks are significant because of how they enable and relate to peak friction loads. Friction loads will not occur without forceful contact. In fact, friction loads can rise only to a certain maximum value directly dependent on the magnitude of the perpendicular loading. To be precise, friction loads can rise to a maximum value equal to the perpendicular (pressure) load multiplied by the coefficient of friction (COF). At that point, a bit of slipping will occur between skin and sock, or between sock and insole, depending on which interface has the lowest COF.”
He also provides this astute comment “Have you ever known insole material manufacturers to provide COF information relative to their product? How many sock manufacturers have included COF information in their literature? I know of none.”
- Carlson J. The Friction Factor. OrthoKinetic Rev. Published online November 2001:1-3.
2005 Lavery et al (Diabetes Technology & Therapeutics):
Measuring the reduction of shear under the sole of the foot, a new insole with two Teflon layers (GlideSoft) was found to be more effective than three traditional insoles.
- Lavery LA, Lanctot DR, Constantinides G, Zamorano RG, Athanasiou KA, Mauli Agrawal C. Wear and Biomechanical Characteristics of a Novel Shear-Reducing Insole with Implications for High-Risk Persons with Diabetes. Diabetes Technol Ther. 2005;7(4):638-646.
2006 Dai et al (Clinical Biomechanics):
A 3-D finite element model (computational model) was used to determine the ability of socks with different frictional properties to reduce shear stress on the sole of the foot. They found that walking barefoot (no sock) has a higher likelihood of blister/ulcer development than when wearing a sock. Further, wearing a low friction sock “allowing proper sliding in footwear” was able to reduce the shear force significantly. And finally, shear force could be further reduced when wearing a low friction sock with low friction properties against the foot skin and the high friction properties set against the insole, in comparison with wearing a sock with the opposite frictional properties.
- Dai XQ, Li Y, Zhang M, Cheung JTM. Effect of sock on biomechanical responses of foot during walking. Clin Biomech. 2006;21(3):314-321. doi:10.1016/j.clinbiomech.2005.10.002
2006 Carlson (Journal of Prosthetics and Orthotics):
This is a highly informative and must-read article. Link here. Here’s an excerpt of the abstract:
“Walking, running, and many other activities involve movements of skeletal elements relative to surfaces such as shoe insoles, orthoses, and prosthetic sockets. Those relative movements are an inevitable consequence of transferring load through soft tissue and across the skin interface. The loads contain both normal (perpendicular to the skin surface) components and friction (parallel to the skin surface) components. Historically, most instances of skin trauma have been attributed directly to excess pressure and have been dealt with using pressure-management techniques exclusively. Pressure-reduction techniques do often lead to some improvement. However, the assumption that those problems are directly governed by excess pressure is substantially in error, leading to partial solutions and missed opportunities to achieve much higher levels of safe, pain-free function.
Research has established the friction component of repetitive loadings to be the major factor governing how many load cycles a given area of skin can tolerate before the onset of pain and acute trauma. To increase comfortable, pain-free function, the magnitude of friction load peaks applied each loading cycle must be reduced. This can be accomplished by reducing peak normal (pressure) load magnitudes and/or reducing the coefficient of friction (COF) operating between the skin and support surface in the problem area. Friction forces over the vast majority of the loaded skin surface area are useful for stability, suspension, and the transmission of functional forces. Friction creates a problem only in very limited areas. This is the rationale for reducing the operative COF in problem areas only.”
- Carlson JM. Functional Limitations From Pain Caused by Repetitive Loading on the Skin: A Review and Discussion for Practitioners, With New Data for Limiting Friction Loads. J Prosthetics Orthot. 2006;18(4):93-103.
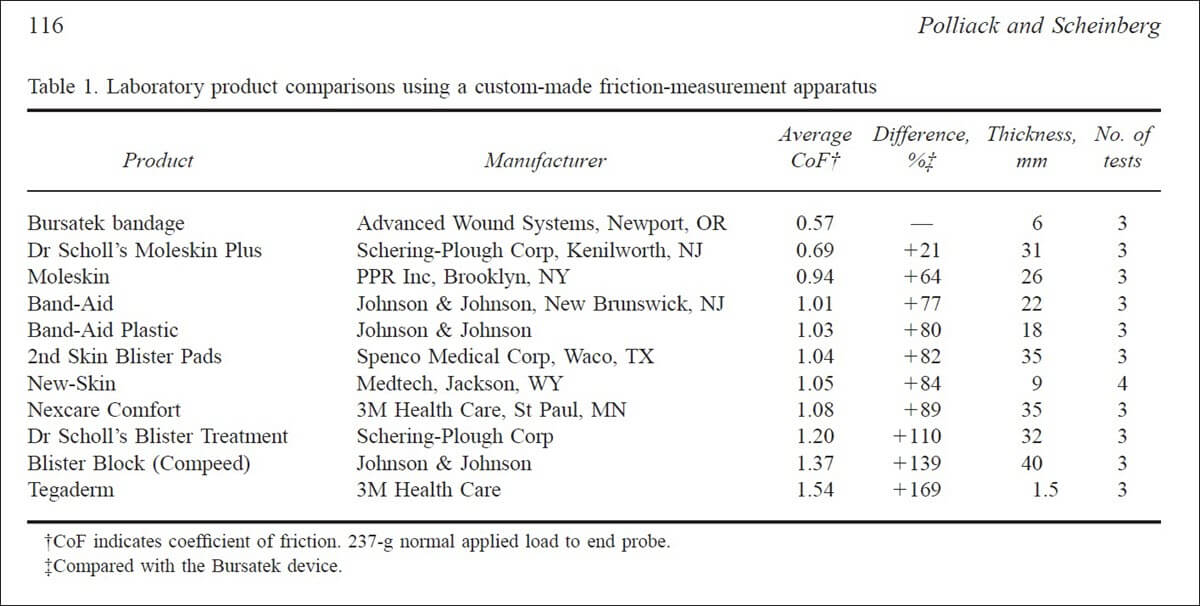
2006 Polliack and Scheinberg (Wilderness and Environmental Medicine):
Blister research of a different kind, Polliack and Scheinberg tested a low COF bandage material, called Bursatek. In fact, the aim of this new dressing was to reduce blister-causing shear in a treatment scenario.
- Polliack AA, Scheinberg S. A New Technology for Reducing Shear and Friction Forces on the Skin: Implications for Blister Care in the Wilderness Setting. Wilderness Environ Med. 2006;17:119.
Blister Research 2010 onwards
2010 Richie (Podiatry Today):
A very readable literature review of how to manage friction blisters and the blister research findings to date. Richie describes blister causation as a tearing within the epidermis as a result of repeated shear stresses. “Frictional forces resist movement of the skin when an external force is acting on the foot to push it in a forward-backward or medial-lateral direction. These forces are known as shear forces. These forces cause the skeletal segments of the foot to move out of synch with the overlying soft tissue and components of the shoe.” This description of skin and bone moving out of sync is such a good one and I believe should be used for a new paradigm for blister causation.
Another good quote highlighting the misconceptions around blister causation and the lag in the mainstream understanding of what to focus on in preventing them: “With such a high incidence and potential for disability, one would think that the prevention of friction blisters would be better understood. Yet few research studies have been published on this subject in the past 20 years. As a result, many myths continue to be propagated regarding the prevention and treatment of friction blisters.”
Another must-read article!
- Richie D. How To Manage Friction Blisters. Pod Today. 2010;23(6):42-49. https://www.podiatrytoday.com/how-to-manage-friction-blisters
2010 Yavuz and Davis (Journal Of The American Podiatric Medical Association):
Tested 3 groups of 11 subjects to find the blister-sufferers exhibited larger pressure and shear stress magnitude than the two control groups.
- Yavuz M, Davis BL. Plantar shear stress distribution in athletic individuals with frictional foot blisters. J Am Podiatr Med Assoc. Published online 2010. doi:10.7547/1000116
2010 Yavuz (Lower Extremity Review Magazine):
Yavuz reminds us that the frequency of shear forces under the foot are twice that of vertical force (pressure) due to both braking and propulsive forces under our feet with each step.
- Yavuz M. Plantar shear: Casting light on ‘dark matter/ Lower Extremity Review Magazine. Published May 2010. Accessed January 2, 2021. https://lermagazine.com/article/plantar- shear-casting-light-on-dark-matter
2011 Carlson (The Academy Today):
Carlson discusses the importance of minimising skeletal movement and friction in order to reduce shear at amputation stumps. In other words, this reduces the chance of skin breakdown. He also provides the data (table below) to highlight the COF of many materials used in orthotics and prosthetics.
In addition, this quote: “In discussing the forces acting upon the surface of the skin, the terms ‘friction force’, ‘shear force’ and ‘traction force’ are, as used in the medical literature, essentially the same. The term ‘shear stress’ is a bit different because it refers to force per unit of area. The medical literature has been a little loose in the usage of these terms, but that has not caused any significant misunderstanding.”
I have to disagree with this statement. I’m sure those well-versed in the science of physics can successfully negotiate these subtleties. However, for the average person (myself included) does not, this ‘looseness’ only adds to the difficulty in understanding and conveying an accurate message. Not only does it not help practitioners understand the definitions and roles of friction and shear, it’s even less helpful to mainstream media.
- Carlson J. The Mechanics of Soft Tissue Damage: Removing the “Teeth” from the Rub. Acad Today. 2011;7(l):5-7.
2012 Scherer (Podiatry Management):
An excellent review recognising our blinkered focus on pressure management at the expense of friction management in the prevention and treatment of shear-related skin injury, specifically foot ulcers. “Increased friction can make a small vertical load very destructive to skin.”
- Scherer P. The Case For Friction Management. Pod Manag. Published online September 2012:111-116. Accessed January 2, 2021. www.podiatrym.com
2012 Antokal et al (National Pressure Ulcer Advisory Panel):
This Advisory Panel update discussed why the reference to ‘friction’ as a factor in pressure ulcer development was eliminated. The definition changed from “localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear and/or friction” to “localized injury to the skin and/or underlying tissue usually over a bony prominence, as a result of pressure, or pressure in combination with shear.”
It also elaborated on static versus dynamic friction as it pertains to the development of shear. As mentioned earlier, I feel that an understanding of static friction and dynamic friction is helpful in understanding the role of friction in shear-related skin damage, including blisters.
- Antokal S, Brienza D, Bryan N, et al. Friction Induced Skin Injuries – Are They Pressure Ulcers? A National Pressure Ulcer Advisory Panel White Paper.; 2012.
2013 Hashmi et al (Skin Research and Technology):
This was an experimental foot blister research paper – one of the few since the mid nineteen hundreds. Blisters were produced on the back of the heel of 30 volunteers and local temperatures measured before, during and after. Temperature at the moment of blister formation increased by a median of 5.1 degrees Celsius (1.7 – 9.9 degrees Celsuis) compared to baseline temperatures.
“We assumed that heat and temperature change generated by pure surface friction was short lived, i.e. dissipated within a few seconds. This was visually apparent on live thermal imaging footage during pilot testing. Since the skin temperature increased after repeated applications of load it is reasonable to assume that a physiological inflammatory response was initiated and responsible for the recorded skin temperature increases. This demonstrates that our method quantified the pre- and post-blister physiological inflammatory changes that occur in response to external loads. Also, that these temperature changes were not due to superficial frictional heat nor changes in environmental temperature (for up to 30 min post blister).”
A year later, Kirkham et al used a temperature change of 3 degrees Celsius to indicate imminent blister formation, quoting Hashmi’s results. “The 3 degree Celsius threshold was based on prior research that identified this as the temperature change indicative of imminent risk of blister creation.” I assume they based this on the interquartile range from those 30 participants which was reported as 3.5 degrees Celsius.
- Hashmi F, Richards BS, Forghany S, Hatton AL, Nester CJ. The formation of friction blisters on the foot: The development of a laboratory-based blister creation model. Ski Res Technol. 2013;19(1).
2013 Krabak et al (Current Sports Medicine Reports):
A disappointing definition of the mechanism for blister formation is mentioned in this discussion on injury and illness in ultramarathon. “Understanding the mechanism of a friction blister injury can help in addressing prevention. The main aetiology is the repeated action of skin rubbing against another surface. As the external contact of either sock or footwear moves across the skin, the frictional force opposes this movement. When horizontal shear forces overcome this resistance, repeated sliding as a friction point causes exfoliation of the stratum corneum and erythema in and around this zone.”
Rubbing is not required for shear. In fact, shear peaks in a state of static friction (no rubbing)!
- Krabak BJ, Waite B, Lipman G. Injury and Illnesses prevention for ultramarathoners. Curr Sports Med Rep. 2013;12(3):183-189. doi:10.1249/JSR.0b013e3182913c98
2013 Rushton (The Advanced Guide To Blister Prevention):
As my first significant writing, albeit online, this ebook highlights the blister research to date and how it is “shear distortions” that cause foot blisters, not rubbing, or heat. It also discusses the four main requirements previous researchers have highlighted as determinants for blister-causing shear, namely: skin type, a high COF (friction level and pressure); moving bone; and repetition. My aim was to highlight how, in order to prevent blisters effectively, one must understand the cause accurately. It goes on to discuss the mechanism by which each prevention strategy works.
Significantly, in this ebook, a discussion with Marty Carlson is mentioned regarding how preventive blister taping works: “Although not described in the literature, it is plausible that tapes reduce shear at discrete locations due to the fact that they’re adhered to the skin. Just as cushioning spreads the vertical load over a larger area to reduce peak pressure, because tape is adhered to the skin, does tape spread the ‘pull’ of the horizontal load over a larger area to reduce peak shear distortion per unit area of skin? In other words, by spreading the shear load, shear per unit area of skin will be less (Carlson, 2013: personal communication).”
- Rushton R. The Advanced Guide To Blister Prevention [2013]. http://www.blister-prevention.com/advanced-guide-to-blister-prevention. Published 2013.
2014 Yavuz et al (Journal Of Biomechanics):
Temperature increase was found to be only a moderate predictor of peak shear stress on the sole of the foot. “Only a moderate linear relationship could be established between the plantar stresses and peak plantar temperature increase. Although a moderate correlation existed between peak shear stress and change in temperature (r=0.78, p=0.002), the location of peak temperature change could not successfully predict the location of peak shear stress (23% accuracy).”
- Yavuz M, Brem RW, Davis BL, et al. Temperature as a predictive tool for plantar triaxial loading. J Biomech. 2014;47(15):3767-3770. doi:10.1016/j.jbiomech.2014.09.028
2014 Lipman et al (Wilderness & Environmental Medicine):
Regarding tape use in preventing blisters, these researchers found paper tape was not protective of blisters in an ultramarathon situation.
- Lipman GS, Ellis MA, Lewis EJ, et al. A Prospective Randomized Blister Prevention Trial Assessing Paper Tape in Endurance Distances (Pre-TAPED). Wilderness Environ Med. 2014;25(4):457-461. doi:10.1016/j.wem.2014.06.013

2015 Yavuz et al (Diabetes Care):
Not specifically foot blister research, but rather diabetic foot ulcers, another shear-related skin trauma. These researchers concluded that it is shear rather than pressure that is the culprit. “This study reports, for the first time in the literature, ulcers occur at peak shear only locations, not overlapping peak pressure locations. Furthermore, more ulcers developed at peak shear locations as opposed to peak pressure locations (50% vs 38%).”
- Yavuz M, Master H, Garrett A, Lavery LA, Adams LS. Peak plantar shear and pressure and foot ulcer locations: A call to revisit ulceration pathomechanics. Diabetes Care. 2015;38(ll):el84- el85.
2015 Hashmi (Measuring The Skin):
This book chapter provides a nice summary of the relevance of moisture to friction levels and resultant shear distortions to the feet.
- Hashmi F. Friction Foot Blisters: The Effect of Hydration on the Risk of Blister Creation. In: Agache’s Measuring the Skin. Springer, Cham; 2015:1487-1494. doi:10.1007/978-3-319-26594-0_145-1
2016 Lipman et al (Clinical Journal of Sports Medicine):
Following the unfavourable results of their paper tape two years previous, this study produced favourable results this time. Paper tape reduced blisters by 40% in an ultramarathon situation.
It’s worth considering that tape completely negates ‘rubbing’ on the skin. Yet there was only a 40% reduction in blister formation with tape in this study. Obviously, there was statistical significance. However, it does highlight the fact that the mechanism can not simply be due to a lack of rubbing on the skin. Shear still occurs within the skin beneath the tape!
- Lipman GS, Sharp LJ, Christensen M, et al. Paper Tape Prevents Foot Blisters: A Randomized Prevention Trial Assessing Paper Tape in Endurance Distances II (Pre-TAPED II). Clin J Sport Med. 2016;26(5):362-368. doi:10.1097/JSM.0000000000000319. PMID: 27070112
2016 Vonhof (Fixing Your Feet):
Vonhof provides a diagram depicting shear as the overall cause of foot blisters and lists some of the contributing factors and prevention strategies.
- Vonhof J. Fixing Your Feet. 6th ed. Wilderness Press; 2016.
2016 Hoffman (Current Sports Medicine Reports):
A great article, Hoffman shares research and opinions similar to my own, published online in 2013 in The Advanced Guide To Blister Prevention. “Blisters result from shear forces within the epidermis causing cell necrosis. The extent of skin shear is influenced by friction at the skin and other interfaces, various skin characteristics, bony movement, and the shear modulus of the foot ware. The number of shear cycles is another factor in the development of blisters.”
Also, this quote is made which echoes those made in The Advanced Guide To Blister Prevention [2013] regarding how preventive blister taping works following my conversation with Marty Hoffman: “Prophylactic taping or patching also may cause a reduction in focal skin shear by distributing shear across a broader area of skin.”
- Hoffman MD. Etiological Foundation for Practical Strategies to Prevent Exercise-Related Foot Blisters. Curr Sports Med Rep. 2016;15(5):330-335. doi:10.1249/JSR.0000000000000297
2019 Rushton (Lower Extremity Review):
Discusses the potential mechanism of action of tape in preventing blisters is spreading shear load.
- Rushton R. Tape Use to Prevent Blisters: Does It Really Do What We Think It Does? Low Extrem Mag. Published online 2019. https://lermagazine.com/article/tape-use-to-prevent- blisters-does-it-really-do-what-we-think-it-does
2020 Rushton (Current Sports Medicine Reports):
Following the 2019 “Tape Use…” article, this one discusses the potential for moleskin working in a similar way – spreading shear load.
- Rushton RJ. Exploring the Mechanism for Blister Prevention Using Moleskin. Curr Sports Med Rep. 2020; 19( 11):451-453. doi:10.1249/JSR.0000000000000768
Conclusion
I hope it is clear that friction blisters on the feet are caused by shear. However, if you feel yourself still magnetised to the old heat – moisture – friction paradigm, please read this article.