Let’s make a start on “How to explain blisters to your patients.” You know, it took me far longer than I care to admit that to understand what shear was. And to really explain ‘what causes blisters’ to my patients. Without falling into the trap of talking about rubbing. So, this presentation is going to take you through my self-education journey and my thought processes along the way as I was learning more and more about friction blisters of the feet. Because, you know, I am far from the sharpest tool in the shed. So, if you too find these concepts difficult to grasp, and to explain, then this might help you – I hope it does.
Types of load
Here we have a picture of different types of load that can be exerted onto an object or a body.
- Compression – That’s like pressure, that’s easy to understand.
- Tension – That’s like pulling an elastic band on either end, that’s easy to understand.
- Bending – I always think of snapping a twig in my hands.
- Torsion – That’s twisting something.
And finally, the one in the middle is shear. This is the one that is relevant to the cause of friction blisters. Unfortunately, this is the one I didn’t really understand.
Part of the reason is images like this – they are on a solid object. But when we’re talking about foot
blisters, we’re actually talking about a viscoelastic body, and so shear has a different impact. There is actual deformation.
Wobbly box
When I was first trying to understand shear, I imagined a wobbly box. Essentially there’s a movement force at the top of the box, and it was important to understand that the bottom of the box didn’t necessarily move in sync with the top of the box – because it was a bit wobbly (viscoelastic). So, you can imagine that at the top of the box is the bone, moving back and forth. And the bottom of the box is the skin surface interacting with all the interfaces external to it.
I understood inertia – you can try an push a heavy box along the floor. Although it won’t move straight away, it often changes shape a little – it deforms (as opposed to something rigid like a fridge – it won’t change shape/deform). Before the heavy but deformable box moves, it has to overcome that friction force between the bottom of the box and the floor. The same thing happens in the foot. The movement force comes form the bone moving back and forth. The friction force is at the skin surface where it interfaces with the groun (for simplicity’s sake, let’s say we’re barefoot), and the deformable box is all the soft tissue layers between skin and bone.
Finger on back of hand
And if you’ve seen any of my videos, you’ve probably seen me do this thing with my finger on the back of my hand. I find this a really good demonstration of what shear looks like, and what it feels like. It’s also really helpful to explain how varying pressure and coefficient of friction has a direct impact on that friction force between the two surfaces. This impacts on the ability of the fingertip to slide across the back of the hand, and therefore the resultant shear deformation in the skin.
Shear deformation is essentially the give in the soft tissue between skin and bone. Shear deformation is what it’s properly called or known as. I often call it shear distortion, just because it was easier for my simple brain to understand. It’s the stretching and distortion within the soft tissues. It’s the give in the soft tissues between skin and bone. It’s not rubbing on the skin surface. This helped me start to explain blisters more effectively, specifically waht causes them, to my patients.
Adapting Martin Hoffman’s image
Back in 2016, Marty Hoffman wrote a summary paper on friction blisters of the feet and he had an image similar to this. I’ve just adapted it so it makes it a bit clearer, anatomically. You can imagine from this image we’ve got the bone (the metatarsal head), we’ve got the skin surface, and then those jagged lines represent the soft tissue between the skin and bone, in a relaxed state. Obviously those soft tissue layers are not aligned vertically, they’re aligned horizontally – this is just a visual representation.
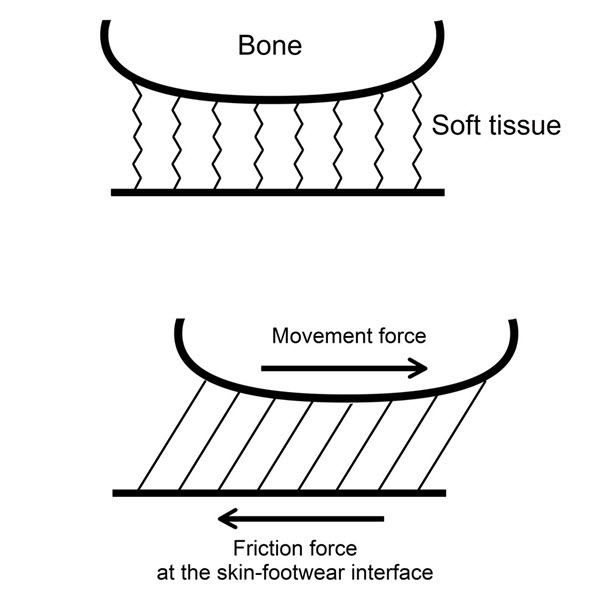
In the lower image you can see as the bone moves one way, the force of friction works in the opposite direction. It doesn’t actually pull the skin in the opposite direction, it simply opposes the movement of the bone in the other direction. The two forces work against one another. The bone is actually moving. And the force at the bottom, at the skin surface, is resisting that. So, there’s an out of sync movement of the bone relative to the skin. That causes all of those tissue layers to shear or translate across one another. I find that’s a really good representation of shear.
Run Smarter Podcast with Brodie Sharp
Not long ago, I was on Brodie Sharp’s podcast and I was doing this on the call with him. And he was in the background with his knuckle or his interphalangeal joint on the desk – and keeping it stuck to the desk, he was wobbling his hand back and forth and feeling that shear within the soft tissues. This was a really insightful representation too. The bone moves back and forth but the skin stays stationary, and you can feel the shear within the soft tissue. So if we think about this as a metatarsal head, as the metatarsal head hits the floor, the bone moves forward. And then, as we go into propulsion the bone moves backward and we have that backwards-directed shear deformation. I found that quite helpful so I wanted to share that with you guys – thanks Brodie!
Here’s how I explain blisters to my patients now
Next, I popped into work on the weekend because I wanted, for the purposes of this presentation, to show you how I explain shear to my patients so that they really understand what’s going on. The hardest thing to get through to our patients is that it’s not rubbing. All of us are hardwired into thinking blisters are caused by rubbing. We don’t fully understand the difference between friction force and rubbing. Let’s watch the video.
I encourage you to try this next time you need to explain blisters, and any other shear related skin injury (that’s blisters, callouses and ulcers, by the way). This leads into an extended conversation about how pressure and coefficient of friction impact the magnitude of shear, and how various blister prevention strategies work:
- Minimise the coefficient of friction
- Minimise Pressure
- Use shear-absorbing materials
- Spread shear load with adhesive products
- Change the way bones move
Getting the blister conversation started
Often, the hardest thing to do is to get that blister conversation started. And it’s difficult to not give the impression that it’s all about rubbing. The cause of blisters isn’t rubbing on the skin, it’s more like rubbing under the skin. This demonstration that I’ve just shown you, that I do every day in my clinic, helps explain blisters so your patient can see and feel the difference. As soon as they realise it’s different to what they thought, they’re more open to your recommendations on how best to prevent their blisters.
Skin anatomy
When we think about repetitive shear and we’re thinking about the blister injury, the injury is a mechanical fatigue. It’s a mechanical fatigue in the epidermis. Specifically, within the stratum spinosum. What I imagine in my mind’s eye when I think about shear is, I think about the bone moving and the skin staying still, is all of these cell layers translating across one another to the extent that the stretch in those little green connectors called desmosomes allow. They’re all put on stretch, back and forth. And depending on the magnitude of that stretch, or depending on how repetitive that stretch is, determines when the mechanical fatigue occurs. So, those connectors, they fatigue and break. That creates a void. Fluid fills that area and it takes up to two hours to form the actual blister. So, once the blister injury occurs, you don’t automatically get a blister straight away – it can take some time for it to fill with fluid.
The new blister causation paradigm
Doug Richie’s and my first paper on blister causation paradigm, proposed two more accurate definitions of what causes blisters. Let’s read them together right now.
Blisters are a tear under the skin surface. Now that’s an important distinction to make because our patients think that they’re caused by rubbing that creates a superficial-to-deep wear injury. This is incorrect. That describes an abrasion.
Blisters are a tear under the skin surface caused by the skin and bone moving out of sync. As the bones move within the foot with each step (which is completely normal and that’s the way it has to be) the skin does not immediately follow. And so the soft tissue’s located between the skin surface and the bones are made to stretch and distort. This is called shear deformation. If there is too much shear, in either magnitude, or duration as in repetitions, a tear develops within the layers of skin which later fills with fluid to form the actual blister.
And then there’s the definition suited more to podiatrists and other health care and sports medicine professionals. Blisters are an intra-epidermal tear (so again, they’re not a superficial-to-deep wear injury, they’re tear within the epidermis) caused by repetitive shear deformation. During ambulation, muscles pull the bones of the feet while high friction forces between the foot skin, footwear interfaces and the ground, maximize efficiency for push-off. It’s actually quite normal for there to be high friction external to the skin surface. It’s by design. We need that for the mechanical efficiencies of gait (braking, propulsion, changing direction), so gait is energy-efficient.
So, if we think about the skin-sock interface, the sock-shoe interface, and then the shoe-ground interface, everything is really designed to stay in stationary contact, while the bones do their thing moving back and forth. And it’s the soft tissues between the skin and bone that take up that differential. That’s the shear deformation. It’s the motion of bones relative to stationary skin creates shear deformation within the tissues beneath the skin surface. Repetitive shear deformation results in mechanical failure or tearing within the stratum spinosum layer of the epidermis which later fills with plasma-like fluid to create the actual blister.
I hope that makes a bit of sense. In the second paper on the critical assessment of current prevention strategies, we’ve got two images that explain where prevention can be implemented. The first picture shows the different levels of bone, soft tissue and external to the skin surface. The second one, the chart is my favorite. I think this really explains blister prevention mechanisms in a really good way.
Blister Prevention Office Hours Q&A
QUESTION 1: If you could boil it down to three things for prevention, what would they be?
QUESTION 2: Best way to prevent blisters/identify hot spots?
QUESTION 3: How can a sports person prevent blisters?
QUESTION 4: Treatment for athletes?
QUESTION 5: How to deal with a ‘growing’ blister?
Is it time to up your blister management game?
Here’s where to go for the best resources and advice to help you explain blisters better to your patients and clients.
🚩 Our Blister Prevention Pro site – you’re already here, so take a good look around.
🎓 Blister Prevention University specifically for podiatrists, sportsmed professionals, educators and anyone involved in footwear design, manufacture and sales.