Today we are going to be talking about sweaty feet.
- Relevance to blister formation
- Sweat gland anatomy & physiology
- Normal foot sweat secretion
- Regional differences
- Hyperhidrosis
- Management/treatment
- Relevance to blister formation
Relevance of foot sweat to blister formation?
Quite simply, even mild to moderate hydration levels of the feet are known to increase skin friction and the likelihood of blisters. This is a snapshot of research and papers that support that. One that I’ll draw your attention to is if you were on last month’s call, we looked at the Hashmi study where they produce blisters on the posterior heel. The same set of researchers basically replicated that study, but this time they had one foot in a bucket of water, and one foot not (it remained dry), and they applied the same repeated shear load to both. What they found was that the rate of temperature change in response to that repeated shear loading was significantly greater on the hydrated skin compared to dry skin. From their previous research, we know that this temperature increase can be used to indicate imminent blister formation. So, the wetter your skin (as opposed to dry), the sooner you’ll get blisters with the same amount of shear load.
In terms of mechanics, where does friction come in? Friction is the force that exists between the interfaces or the materials external to the skin surface. So we’re talking at the skin-sock and sock-shoe interfaces. So if friction force is high, it keeps everything stuck together while the bones are moving back and forth in the foot as part of normal mechanics. So the bones are moving back and forth, the skin staying still, and all the soft tissues in between allow that to happen by undergoing shear deformation. If those fiction levels are high, the skin stays still for longer; and given the bone has to move a certain amount, the magnitude of shear deformation is going to be larger when that friction force is high. But if we can reduce that friction force, then as that bone moves the exact same amount, then the skin is able to move in sync with the bone at an earlier moment in that individual shear distortion, thereby reducing the magnitude of that shear distortion. Foot sweat is what increases friction force, compared to dry.
Sweat gland anatomy and physiology
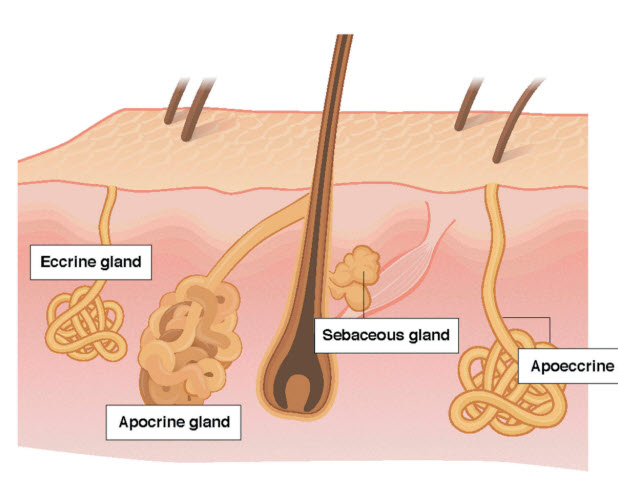
Sweat gland comparison, from Baker, L. (2019). Physiology of sweat gland function: The roles of sweating and sweat composition in human health. Temperature. 6(3), p 211-259
There are some sweat glands that are irrelevant to the feet, so just quickly:
Apocrine sweat glands (not on the foot)
- Specific regions of the body (axilla, breasts, face, scalp)
- Larger than eccrine
- Open into hair follicles instead of directly onto skin surface
- Present from birth but secretory function does not begin until puberty
Apoeccrine sweat glands (not on the foot)
- Develop from eccrine sweat glands at ~8 to 14 years
- Not on the dorsal or plantar foot
Sebaceous glands (not on the foot)
- Not a sweat gland
- Associated with hair follicles
- Widespread, particularly scalp, forehead, face, anogenital area
- Hormonal control
Eccrine sweat glands
The sweat glands relevant to the feet are the eccrine sweat glands:
- On glabrous & non-glabrous skin
- Most numerous (~2–4 million)
- Highest densities on palms and soles (~250–550 glands/cm2)
- Responsible for the highest volume of bodily sweat
- Functional at ~2–3 years of age
- Total number is fixed
- Sympathetic innovation
- Respond to thermal and psychological stimuli
Sweat gland cells
If we have a real quick look at the sweat gland cells, they can be basically divided into the duct (the straight bit that takes the sweat to the surface of the skin); and the secretory coil (the big ball of wool at the bottom).
The bits that I’ve circled in blue are the duct cells. Their primary function is the reabsorption of sodium and chloride ions as the sweat passes up towards the skin, so that the sweat that is finally secreted on the skin is hypotonic.
And if we look at the secretary coil cells, there are three types of cells. There are clear cells – they’re the ones that actually produce the sweat. There are dark cells – we don’t really know what they do. And there are myoepithelial cells (the clue is in the name) – they have a contractile function.
Eccrine sweat glands primarily respond to thermal stimuli; particularly increased body core temperature, but also skin temperature and increased skin blood flow; so basically, thermoregulation. Thermal sweating is mediated predominantly by sympathetic cholinergic simulated stimulation. So we’ve got this sympathetic post-ganglionic neuron; it gets to the clear cells; it releases acetylcholine and that binds to the muscarinic receptor on the clear cell. So it’s the release of the acetylcholine that kick-starts sweat production.
Eccrine glands also secrete sweat in response to adrenergic stimulation but to a much lesser extent. So that’s basically the fright or flight response. In addition, eccrine sweat glands respond to non-thermal stimuli related to exercise; this is in reference to the fact that we know people that are fit and exercise a lot, they sweat more and sooner than people that don’t exercise a lot. So you can say that their thermoregulation. is more effective.
A quick summary so far:
- Sweating is mainly for thermoregulation. But it’s also relevant to the fright or flight response. And also non thermal stimuli relating to exercise.
- The dorsum of the foot has a much lower gland density than the plantar surface and it’s primarily responsible for thermoregulation.
- The plantar service has a much higher gland density and it responds to emotional as well as thermal stimuli.
So if you had to say right now which part of the foot sweats more – the dorsal surface or the plantar surface, which would you say? I’d say the plantar surface.
Well, you might be in for a surprise…
How much does each foot sweat?
Carlson mentioned a quick pilot study that they did in his 2006 paper. They got fresh socks from three runners and the moisture content was 15%, 23% and 31%. So he suggested that if we’re interested in what’s going on in the shoe in terms of the moisture from foot sweat in the sock, we should be looking at a moisture content of the sock of about 25 to 30%. The graph on the right is where they got a cotton sock and they gradually increase the water content from zero to 100%; and you can see the differences in the coefficient of friction on the y axis here.
If we look at what happens as the sock gets wetter, PTFE (which is the Engo patches or Shearban) the COF remains relatively constant no matter how wet the sock gets, with a coefficient of friction of about 0.2. The yellow line is Poron. It increases sharply to about that 25%-30% mark, then at levels off; and then it increases again at around 70%. Plastazote is relatively stable from around 0.45 to 0.5. And Spenco increases for the first half and then kind of levels off for the second half. Now, we know Spenco has a good blister prevention effect – that research has been done in terms of blisters and calluses. So from this data, you would probably question whether it’s main mechanism is coefficient of friction reduction. Probably I would think it’s more likely to be something else and my best guess would be shear absorption and maybe even pressure management.
How much do the feet sweat? Here are some values from the research:
- 30-50ml per hour (cycling to exhaustion)
- 212-416g per sq metre per hour (65-minute uphill walk with a backpack)
- 0.23-0.50mg per cm per min (passive heating ie: at rest)
- 0.3-0.5mg per cm per min (running)
- 0.41-1.20mg per cm per min (cycling to exhaustion)
The first two are from 2006 to 2007. The others are from a subsequent paper that was similar to the first two, and we’ll talk about in a minute (see references).
Foot sweat rate: regional differences
From what I understand, these Taylor (2006) and Fogarty (2007) papers are the first two that really looked closely at regional differences on the feet. Both of them find that the dorsal aspects sweats a lot more than the plantar aspect; around about 70:30. Nigel Taylor is from the University of Wollongong and he and his team have done a lot of work in this area, publishing a lot of data. And the Fogerty is a UK study.
Let’s have a look at some pictures from the Taylor study. They used these sweat capsules on 5 areas of the feet:
- 3 dorsal aspect
- 1 lateral aspect (I’d describe it as dorsolateral)
- 1 plantar aspect
The heating method was one-legged cycling. So what they did was that both feet were “nude” or uncovered. One foot was doing the cycling and the other one had all these capsules on it for measurement.
Let’s have a look at what they actually found in terms of sweat rates. The top graph is the average across the whole trial; the bottom one is the last 15 minutes. Either way. they’re kind of similar. So the dark black bar which is the biggest, that’s the forehead. So first we can tell that the feet sweat less than the forehead. Second thing that is interesting is the last little ones are for the sole of the foot capsule. The others were the dorsal and dorsolateral capsules. So, there you go.
Now, I was keen to just see if there was more information. Because I found it hard to believe that the plantar surface doesn’t sweat more than the dorsal surface. So if you read more research, we’ve got this combined paper. The one on the right with the same capsules is from Nigel Taylor and his crew at the University of Wollongong and you can see that they had more capsules on the feet (11 all up). And the one on the left was from the UK and they used absorbent patches that stuck to the skin. You can see that it covers about 90% of the foot.
The idea was that they wanted to pool the data. So although they were using different methodologies, they found a way to make it so the results could be pooled and be more meaningful due to the larger number of subjects.
The one on the left was absorbent patches collecting the foot sweat. The subjects were running at different intensities. And for the study on the right, there were two heating mechanisms: passive heating at rest; they wore what I imagine is something like a wetsuit where they pump hot water into it to heat the skin. And then after they did that, they performed that one-legged cycling thing again. Two differences between the two studies to note are, the one on the left were wearing shoes, and the one on the right was barefoot.
Results
Results from both laboratories are in agreement:
- The feet sweat less than the forehead
- Males secreted more than twice the volume of sweat as females at the same relative work rate
- Highest local sweat rates were observed from the medial ankles
- The dorsal foot sweated substantially more than the plantar areas.
- Both genders demonstrated a non-uniform sweat distribution, though this was less variable in females
- Sweating on the plantar side of the foot was uniform
Another finding was that wearing shoes (absorbent patches) limited the increase in foot sweat production, while the sweat rate of uncovered feet (sweat capsules) kept increasing with work and thermal load. This is what they call hidromeiosis. Essentially the skin swells due to the excessive hydration and that closes off the sweat ducts and blocks sweat secretion.
This is a different study. Fourteen females performed low intensity running with nude feet, and low and high intensity running with shoes. Foot sweat rates were measured at 14 regions using the absorbent patches and what they found was the barefeet sweated 22% more than those that were in shoes – that’s another example of hidromeiosis.
The highest foot sweat rates were observed at the medial ankle and dorsal regions. Lowest sweat rates were at the toes. And interestingly, and significantly for anyone who is having a hard time believing the plantar surface of the foot sweats less than the dorsum “Perceptions of wetness and foot discomfort did not correspond with regions of high sweat production or low skin temperature but rather seemed dominated by tactile interactions caused by foot movement within the shoe.” So even though the dorsal surface is sweating more, you just feel it more on the plantar surface.
Another study: this one was an non-thermal stimulus. Subjects performed mental arithmetic in a temperature controlled room, with psychological sweating evaluated from nine sites. They used the ventilated capsules for this one. The results showed sweating was evident from three glabrous sites (glabrous means not hairy ie: the plantar/palmar surface). However, significant sweating was evident from two non-glabrous (hairy surfaces). There is thought that psychological stimulates sweat only on the glabrous skin, but these results refute that: “These observations further refute the proposition that psychological sweating in humans is restricted to glabrous (plantar and palmar) skin surfaces.
One interesting thing that was mentioned was that “Most of the variability in regional and whole body sweating rates within and between individuals is due to differences in sweat secretion rate per gland, rather than the total number of active sweat glands”. So that kind of makes sense because we’ve got high density sweat glands on the plantar surface and yet that’s not the part that sweats more.
Hyperhidrosis
Hyperhidrosis is a disorder of excessive sweating for no good reason. It’s not people that sweat a lot when they exercise; and it’s not people that sweat a lot when they’re stressed out. It’s people that sweat profusely in a resting state with no thermal or psychological stimuli. That is the definition of hyperhydrosis.
So, it’s a disorder of excessive sweating beyond what the body uses for homeostatic temperature regulation. It’s due to the overstimulation of cholinergic receptors on eccrine sweat glands. The acetylcholine negative feedback loop is likely impaired. And interestingly, eccrine sweat glands appear normal in size and number but the sympathetic ganglia are usually larger, in people with hyperhidrosis.
Hyperhidrosis can be classified as either primary or secondary. Primary presents earlier in life; the aetiology remains unknown and; genetic factors are thought to be involved, but it’s not that well understood. Secondary hyperhidrosis is usually the effect of medications or systemic disorders.
Some interesting facts about hyperhydrosis:
- It’s estimated that 3% of the US population suffers with this disorder.
- It affects all races but has the highest incidence in Japanese.
- Developing segmental or localized hyperhidrosis is relatively rare
- The rare cases of unilateral hyperhidrosis tends to be more common on the right side of the face or arm with anhydrosis on the left side.
Moisture Management / Treatment
We can obviously use socks to manage foot sweat. Moisture wicking obviously makes intuitive sense. So if there is a moisture wicking function, it takes moisture away from the skin surface, so it can be evacuated into the shoe environment and then through the shoe into the atmosphere. Which moisture wicking sock works best? Who knows. Does moisture-wicking work better than a wool sock? Who knows. We don’t know; the research isn’t there. Merino wool is used in a lot of socks. We know that wool has the ability to absorb moisture within the fibre, which moisture wicking synthetic fibres don’t.
Toe socks obviously give us a moisture management function at the interdigital space where normally there is none; normally it’s a skin-skin interface, but now we put two sock layers in there.
We know that thick socks work better than thin socks. We know this from the Herring and Richie studies from the early 1990s. Comparing cotton and acrylic, it was a thickness that mattered most in terms of blister protection. We could assume that the thickness was required for a moisture-wicking function. But who knows, it could have been something else related to its thickness. So it could have been a pressure reduction strategy or could have been by a shear absorption mechanism. But either way we kind of know that thick socks work better than thin. And of course change out of wet socks. Even just once in the middle of the day can help a lot in managing moisture. Ventilated shoe uppers obviously aid moisture escape much better than Gore-Tex.
Astringents decrease sweating by denaturing keratin, occluding the pores of the sweat glands. So foot sweat is still produced, it just can’t get out onto the skin surface. Unfortunately, the effect is very short-lived.
Aluminium chloride hexahydrate 20% for example, DriClor is an over-the-counter antiperspirant. I had a quick look online this morning and you can buy it on Amazon and eBay (in Australia), but I couldn’t find it in any of the major online pharmacies. So, I don’t know what the go is there, but it’s available. The idea is you use it for three to four nights in a row and then nightly as needed. Skin irritation can occur in patients often becoming intolerant of it in the long term.
Iontophoresis is a setup where you put a bit of water (tap water) on these pads, you stand on them, they plug into the wall and they put an electric current through the water. It doesn’t hurt, it’s just a bit of a tingle. The mechanism isn’t well-understood. Compliance is relatively low with this. It costs a little bit to set up but I think all the gear lasts a long time. I know of a couple of people that have used this – one finds that it works really. It’s a bit of an ordeal – it’s not just ‘treat it once or every day for a week or a month and then you’re done’. You go intensely for a little while and then you sort of spread out the treatments over time.
Oral anticholinergic medications include Glycopyrrolate, Oxybutynin, Benztropine and Propantheline. Side effects can include dry eyes, dry mouth, urinary retention, and constipation. The product on the right isn’t an oral, it’s a cloth used mainly for the axilla, but it uses the same ingredient as one of the orals (Glycopyrrolate). I’m not sure if you can get it in Australia, but it’s definitely in the US it’s on prescription.
Botox injections can be done. The decreased perspiration can last from 6 to 24 months, so that’s pretty decent. Essentially, it blocks the release of acetylcholine so foot sweat isn’t even produced. So if we block the release of the acetylcholine, the clear cell just can’t produce the sweat. And lastly, sympathectomy and local excision, which would be done even less than Botox I would suggest.
The consensus is that “no treatment works reliably and recurrence is common”.
Wrapping up
So that basically wraps it up.
We’re not going to have time for Q&A in terms of the questions submitted earlier – we got some really good questions during the week, so we’ll do a full 30 minute Q and A next month.
References
- Kirkham S, Lam S, Nester C, Hashmi F. The effect of hydration on the risk of friction blister formation on the heel of the foot. Skin Res Technol. 2014;20(2):246–253.
- Baker, L. (2019). Physiology of sweat gland function: The roles of sweating and sweat composition in human health. Temperature. 6(3), p 211-259
- https://www.ncbi.nlm.nih.gov/books/NBK459227/
- Carlson, J.M. (2006). Functional Limitations From Pain Caused by Repetitive Loading on the Skin: A Review and Discussion for Practitioners, With New Data for Limiting Friction Loads. JPO Journal of Prosthetics and Orthotics, 18, 93-103.
- Taylor N et al. The sweating foot: local differences in sweat secretion during exercise-induced hyperthermia. Aviat Space Environ Med. 2006;77(10):1020–1027.
- Fogarty A et al. Regional foot sweat rates during a 65-minute uphill walk with a backpack. In: Mekjavic I et al. Environmental Ergonomics XII: Proceedings of the 12th International Conference on Environmental Ergonomics. August 19–24, 2007, Piran Slovenia. 2007:283–284.
- Smith, C, Machado-Moreira, C, Plant, G, Hodder, S, Havenith, G, & Taylor, N. (2013). Design data for footwear: Sweating distribution on the human foot. International Journal of Clothing Science and Technology, 25(1), 43-58.
- Smith, C, Machado-Moreira, C, Plant, G, Hodder, S, Havenith, G, & Taylor, N. (2013). Design data for footwear: Sweating distribution on the human foot. International Journal of Clothing Science and Technology, 25(1), 43-58.
- West, A. M., Tarrier, J., Hodder, S., & Havenith, G. (2019). Sweat distribution and perceived wetness across the human foot: the effect of shoes and exercise intensity. Ergonomics, 62(11), 1450–1461.
- Machado-Moreira, C. A., & Taylor, N. A. (2012). Psychological sweating from glabrous and nonglabrous skin surfaces under thermoneutral conditions. Psychophysiology, 49(3), 369–374.
- Herring, K., & Richie, D., Jr. (1990). Friction blisters and sock fiber composition. A double-blind study. Journal of the American Podiatric Medical Association, 80(2), 63-71
- Herring, K., & Richie, D., Jr. (1993). Comparison of cotton and acrylic socks using a generic cushion sole design for runners. Journal of the American Podiatric Medical Association, 83(9), 515-522.