We are going to be looking very closely at posterior heel blisters today. Interestingly, this is where my special interest started with blisters.
Here’s what we’ll cover:
- Common (incorrect) understanding
- Relative motion (rubbing) scenarios
- Heel lift
- Heel strike
- Research
- My experience
- How preventions work
- Recap
- Questions
The common understanding of what causes posterior heel blisters
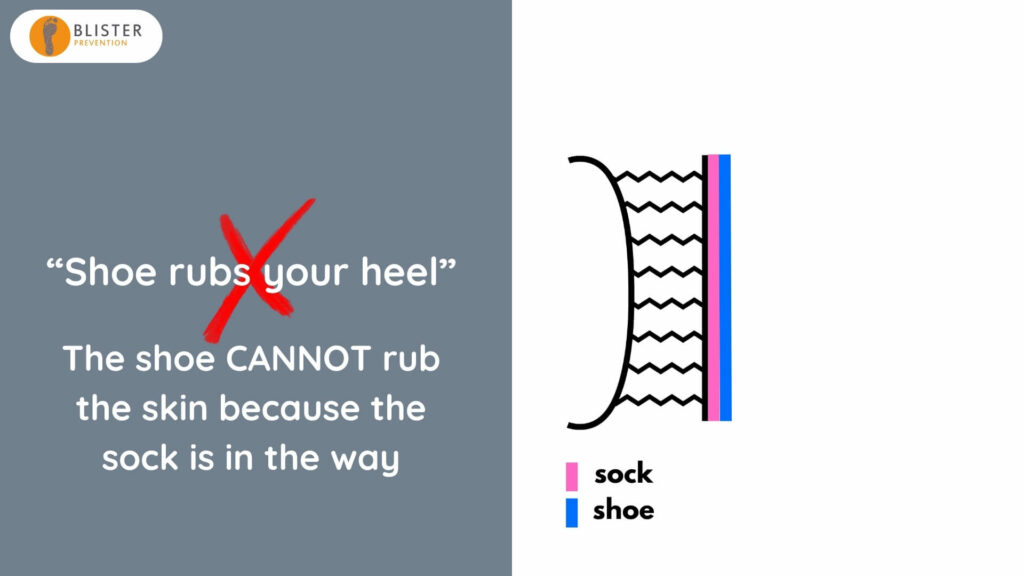
The common, and might I say incorrect, understanding of the cause of posterior heel blisters is that your heel rubs the shoe, or your shoe rubs your heel. Well, if we have a closer look at what’s going on at the posterior heel, we’ve got the posterior calcaneus, the skin surface, and the subcutaneous tissue layers. Obviously those soft tissue layers run parallel with the skin surface.
If we add in the shoe and the sock, it quickly becomes apparent that it’s actually impossible for your shoe of your heel, or for your heel to rub your shoe – because the socks in the way. So what is rubbing what. And is rubbing even important to blister formation? Because we know that blisters are caused by repetitive shear deformation.
Recap – What is shear deformation?
Let’s have a quick recap what shear deformation is. Shear is basically the give in the soft tissues. So as the bone moves back and forth, the skin doesn’t necessarily follow straight away (if at all) and the soft tissue layers have to cope with that differential. So they stretch and distort or deform as a result.
It’s important to remember that obviously the foot is not a block of cement – the bones move within the foot as part of normal function. That’s why skin markers aren’t always indicative of bone position. Unfortunately, shear isn’t readily visible – because it’s happening under the skin surface – it’s happening inside the foot. So that makes it a little bit difficult to visually appreciate.
And you don’t need rubbing for shear deformation to occur. You can see that the skin surface isn’t moving at all, and yet as the bone moves back and forth. The soft tissue between skin and bone is stretching and distorting or deforming and that’s what shear is.
Relative motion (rubbing)
Let’s have a look at some relative motion (rubbing) scenarios at the posterior heel, at both heel lift and heel strike. As the foot moves through mid-stance and it comes towards heel lift, the Achilles pulls on the calcaneus pulling it upwards. If friction levels determine that the skin and the sock and the shoe remaining stationary contact, given that the heel has to move up a certain amount as part of normal function, then it’s the job of the soft tissues between skin and bone to allow that to happen. So they stretch into distort (shear deformation) to allow that to happen.
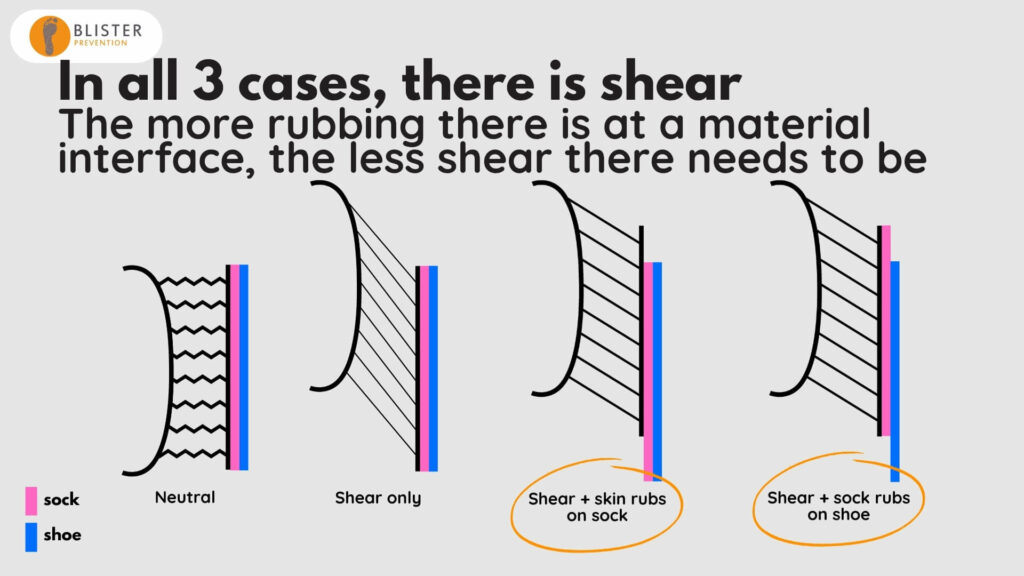
If we compare that to what happens if we have slippage of the skin on the sock, and see what that means for the magnitude of shear deformation, you can see the magnitude of shear deformation has reduced, because the skin has moved relative to the sock. So, as the bone has moved upwards, the skin has been able to move at an earlier moment in time with the bone, and therefore that reduces the magnitude of shear deformation.
Similarly, if we get that slippage between the sock and the shoe, again shear deformation is less, because the skin has been able to move in sync with the bone at an earlier moment in time, thereby reducing the magnitude of that shear deformation.
Let’s look at heel strike. It’s exactly the same but in the opposite direction. As the calcaneus moves down at heel strike, if friction levels determine that the skin remains in stationary contact with the sock, which remains in stationary contact with the shoe, then given that the bone has to move down a certain amount, the soft tissues will stretch and distort (deform) to allow for that to happen.
If we compare that to the magnitude of shear when there is slippage between the skin and the sock, then the skin is released to move in sync with the bone at an earlier moment. Therefore, it reduces the magnitude of shear deformation. And it’s the same if we get that slippage between the sock and the shoe.
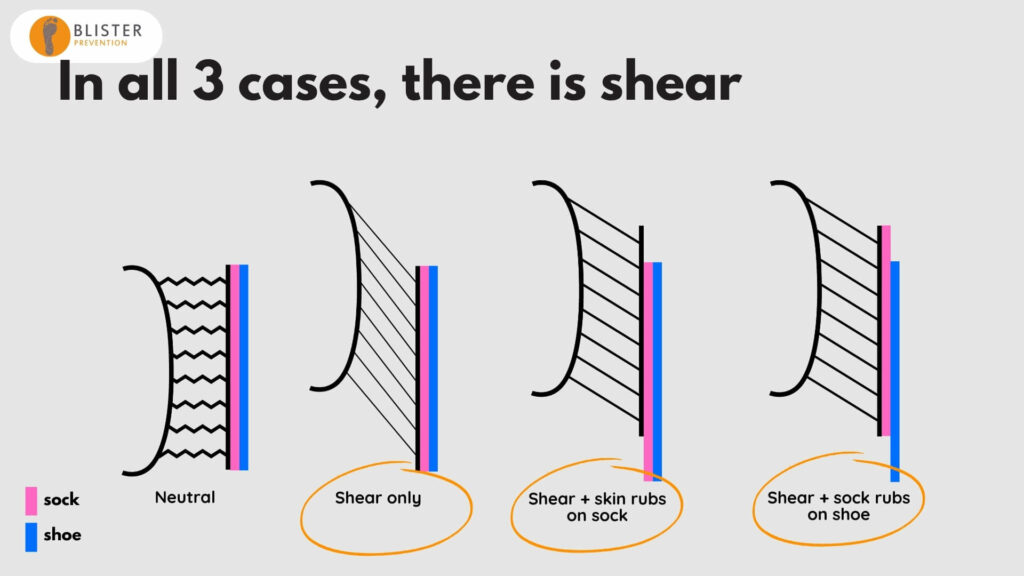
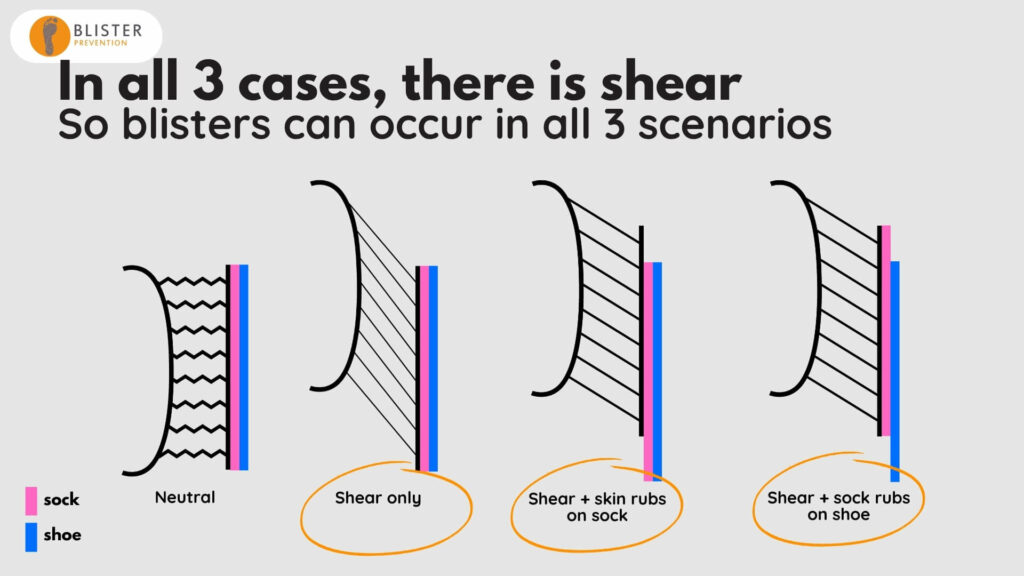
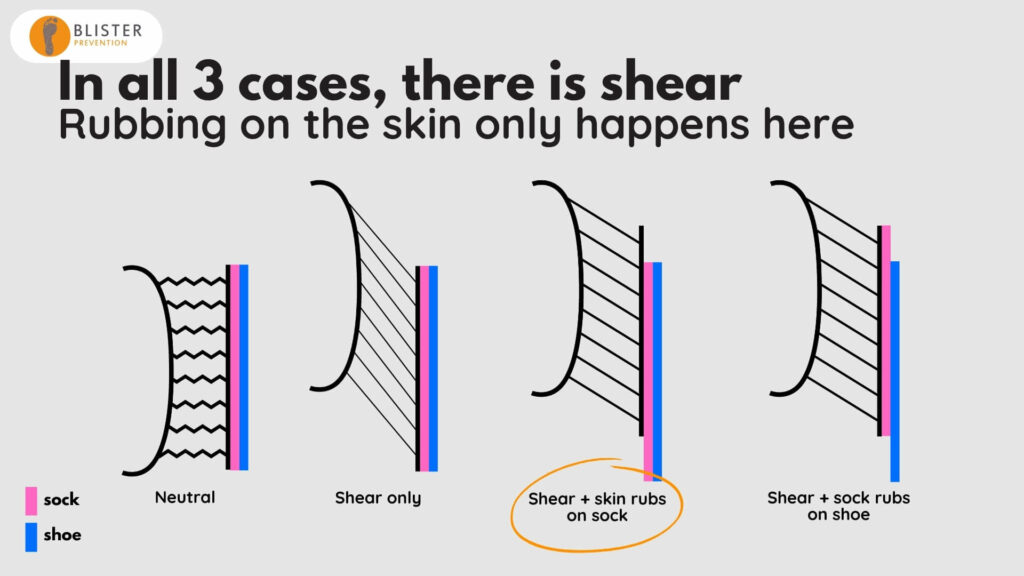
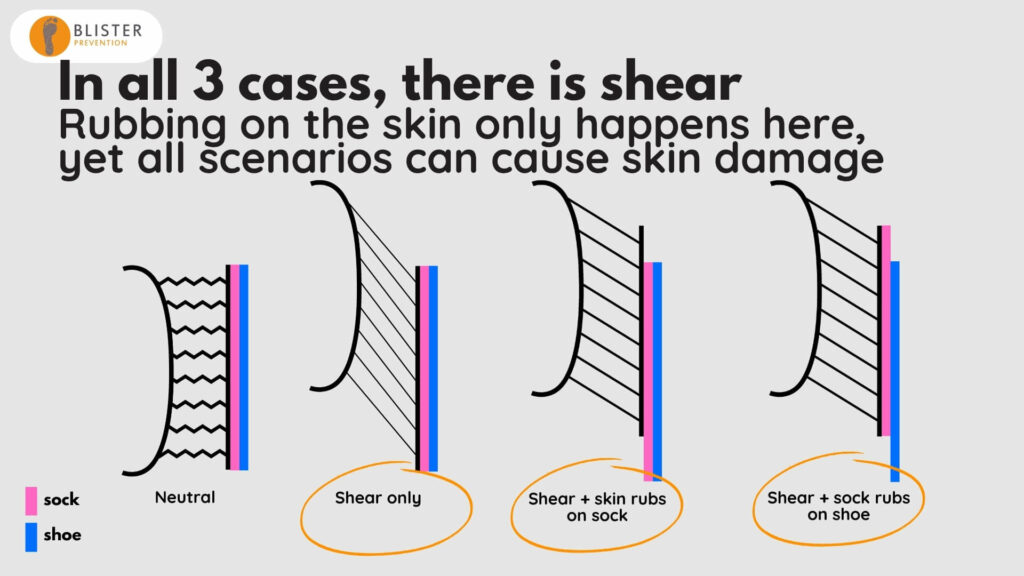
If we look at all three scenarios:
- We have shear deformation in all three. So blisters can occur in all three scenarios.
- Rubbing only happens in one of these scenarios. So if that is a high fiction rub, we risk abrasion damage to the skin, which is a superficial-to-deep where injury.
- Yet all scenarios can cause skin damage. That’s because we’re talking about the skin damage of repetitive shear deformation (not superficial-to-deep wear injury). This type of skin injury is an intra-epidermal mechanical fatigue of the connections between skin cells within the lower part of the stratum spinosum of the epidermis.
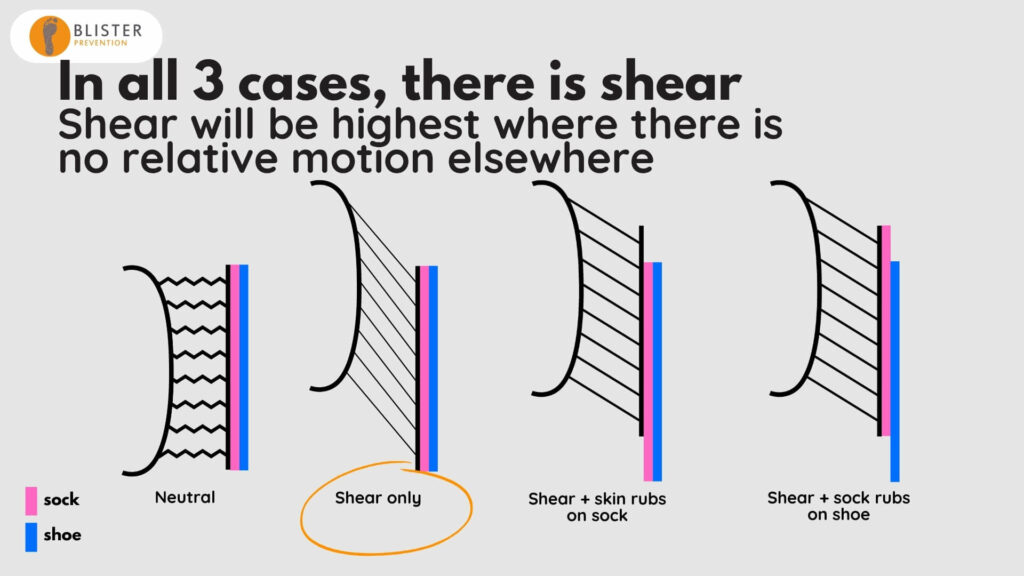
- Shear is highest where there is no relative motion (rubbing) between the skin, sock and shoe.
- And when there is relative motion between either the skin and sock, or the sock in the shoe, then shear deformation is reduced.
If I put a couple of labels in here of actual preventions that fit the bill:
- On the far, right we’ve got Engo Patches. They are a made from a low friction material called polytetrafluoroethylene (PTFE). They’re a self-adhesive sticker that you stick to the shoe, so the sock is able to move up and down very easily over it, thereby releasing the skin to move in sync with the bone at an earlier moment in time, thereby reducing the magnitude of shear deformation.
- Same thing with lubricant but this time between the skin and the sock, so the skin is able to move relative to the sock very easily.
- And if we try and increase friction levels at any of these material interfaces at the posterior heel, like a heel grip or neoprene, then we’re encouraging things to stay in stationary contact and there will be a higher magnitude of shear deformation in the subcutaneous tissues between skin and bone
Rubbing (relative motion) is not the problem
Shear is the problem of blisters
And rubbing is often the solution
As long as it’s a low friction rub. If it’s a low friction rub, it’s a blister prevention strategy. If it is a high friction rub between the skin and the sock then we risk an abrasive injury as well.
Research
Now we’re going to have a quick look at some research. This research was conducted by Farina Hashmi and colleagues in the UK in 2013. They produced blisters on the posterior heel of 30 subjects using this load applicator mechanism. Basically, this jig moved the applicator up and down, and the surface of the applicator was rubber – so it was a high friction material. That created the shear deformation in the skin at the back of the heel.
The authors discuss two things in this paper that I want to highlight. These weren’t the findings of the paper, but they were just two things that were mentioned in the discussion of the topic.
1. “Normal” relative motion
The first was that the heel moves down, relative to the back of the shoe at heel strike, by a whopping 1.5 centimetres. Now that is a lot more than I would have ever thought. I think most podiatrists would think that is a lot and I have to say that, as podiatrists, we aim to make that as little as possible, if any at all. However, 1.5cm is maybe not to be taken as gospel. This 1.5cm was discovered as part of an unpublished pilot study. There’s really no information on how it was conducted. So, I don’t know the number of subjects; I don’t know the type of shoe; I don’t know how it was measured – whether they cut a hole in the back of the shoe, whether they used a skin marker or a bony landmark.
On the surface of it, this seems like a pretty easy research project to do – so if there’s a final year podiatry student looking for a project to do, as long as you’ve got a good camera and video analysis equipment, it would be great to be able to verify that 1.5 centimeters is a “normal” amount for the heel to move relative to the back of the shoe.
2. Bidirectional or unidirectional?
The other thing they mentioned was the majority of shear at the posterior heel occurs as the foot moves down into the shoe after heel strike, and so it is unidirectional. This was just stated; there was no reference. I know that it definitely hurts more at heel strike, than heel lift when you’ve got a blister. So there’s no doubt that there is a lot of shear at heel strike. But how relevant is the heel lift shear event? Is it negligible? This becomes important as we know blisters are caused by a repetitive shear deformation; the “repetitive” part is very important – the more repetitions the sooner blisters will occur. If it is actually unidirectional then that means that there’s one shear episode per step. But if it’s bidirectional, there’s actually two shear episodes in one step – that’s double the shear in terms of repetitions. I don’t kow, but could it be that this is part of the reason why posterior heel blisters are very common.
Anyway, so the heel moves down 1.5cm relative to the shoe at heel strike; and presumably it moves up 1.5cm relative to the shoe at heel lift. And when we say heel, I’m assuming that we’re talking about the skin. Remember, the bone is actually moving up and down more than the skin. Instinctively this 1.5cm up and down seems like a bad thing. But is it? Because we’ve just said that rubbing (relative motion) is not the problem. The thing is you’ve got to focus on is not rubbing, but what that rubbing means for the magnitude of shear deformation. Because if we were laser-focused on preventing rubbing, then we would increase friction force at the back of the heel and have the situation where we’re actually encouraging shear deformation to be larger.
So the moral of the story here is that keeping the skin, sock and shoe stuck together is not the primary aim in preventing posterior heel blisters. We’ve got to focus on the magnitude of shear deformation.
My experience with posterior heel blisters
Posterior heel blisters were my most common blister. I’d get them with walking, not hockey (hockey would give me an edge blister at my first MPJ). I wasn’t aware that my heel was slipping up and down excessively. In fact, I optimized shoe fit and lacing to ensure that that wasn’t the case because my understanding was I did not want my heel lifting up too much because that’s rubbing.
Things that didn’t help were calf stretches. Again. I didn’t want my heel lifting up so much. So I did calf stretches, but I don’t know perhaps I wasn’t tighten the calf muscles. I didn’t think I was, but I was just trying to throw everything at it. I couldn’t find a sock combination that would help.
Things that did help but didn’t help enough included taping. Taping definitely helped. I’d rather have it than not have it, but I would still get blisters under the tape. Firm lacing did help but not enough to keep me blister free. And minimizing heel strike was one thing that I would do once I had a blister, because heel strike was when it was at its most painful. So I would try and affect a forefoot strike or a flat foot strike, which is kind of hard to do when you’re walking for exercise because you can’t really get much pace up. And the thing that helped the most was Engo patches.
Now, I had two conceptual challenges that I had to get my head around.
- The first, I eliminated the rubbing on my skin with tape, yet I’d still get a blister.
- And secondly, the thing that helped the most made rubbing easier.
So that was my confusion and started my whole investigation into understanding blisters better. These are my current walking shoes with their Engo heel patch attached. It’s a polytetrofluoroethylene material, so it’s very low friction. This lets my sock glide up and down on the Engo patch very easily, and that reduces the magnitude of shear deformation at both heel lift and heel strike.
“Friction reduction strategies aim to allow the skin to move in sync with the bone at an earlier moment of time with every step. That’s how they reduce the magnitude of shear deformation.”
HOW PREVENTIONS WORK
Now we are really going to get into the nitty gritty, so strap yourself in. We’re going to look at all the blister preventions that can be applied to the posterior heel, or as many as I could think of, and exactly how they work. We’re going to look at:
- Coefficient of friction reduction strategies lubricants like Engo patches, double socks, moisture wicking socks.
- Pressure reduction strategies like donut pads, cushioning materials and foot strike angle.
- Materials that absorb shear like PelliTec pads, gel materials and padded socks.
- Adhesive materials that we can apply to the foot that spread shear load.
- And ways to reduce sagittal plane motion of the calcaneus.
COF REDUCTION AT THE SKIN-SOCK INTERFACE
Lubricants and moisture-wicking socks are coefficient of friction (COF) reduction strategies that work at the skin-sock interface. Now, it’s easy to understand lubricants; you put Vaseline for example on your skin, that makes it slippery, and so your skin is able to move relative to the sock to affect a smaller magnitude of shear deformation within the foot.
Moisture-wicking socks are trying to negate the high friction effect of moisture on the skin surface. They’re trying to get that perspiration that comes from the skin to move through the sock, so it gets into the shoe and it either absorbs into the shoe materials (like the lining or the insole) or is evacuated into the airspace of the shoe and ideally evaporates through the upper of the shoe. That’s how moisture-wicking socks work.
Now we’ve discussed these two examples, I think that you can appreciate that one makes it more slippery than the other. Lubricants make it slippery. I don’t feel that my foot’s that slippery when I wear a moisture-wicking sock though, even when I’ve been exercising for a while. So, with each strategy we discuss, even if they work by the same mechanism at the same interface, some are more effective than others.
COF REDUCTION AT THE SOCK-SHOE INTERFACE
Engo patches are represented here with the yellow line. So, the yellow Engo patch is adhered to the shoe, so there’s no movement there. Because of the low fiction surface of the patch, the sock is able to move up and down very easily over it. That releases the skin to move inside in sync with the bone at an early moment of time, thereby reducing the magnitude of shear deformation.
COF REDUCTION AT THE SOCK-SOCK INTERFACE
- Now if we have a look at them all together:
- In all three cases, we have soft tissue shear deformation, so blisters can occur in all three scenarios.
- Rubbing on the skin only occurs in one scenario. So abrasion to the skin surface can only happen in one of these situations. It won’t happen if it’s a very low friction rub, but if it’s a high friction rub, you will have the potential for abrasive injury to the skin. Abrasive injury (abrasion) is essentially a superficial-to-deep wear injury.
- Yet all three scenarios can cause skin damage. That’s because we’re talking about the skin damage that occurs with repetitive shear deformation, which isn’t a superficial-to-deep wear injury. It’s a mechanical fatigue within the layers of the epidermis.
- Interestingly, shear deformation will be highest where there’s no relative motion between the skin sock and shoe. Given that the bone has to move up a certain amount, the soft tissues will have to shear to allow that to happen.
- And the more rubbing that occurs at a material interface, the lower the magnitude of shear deformation that has to happen within the soft tissues of the skin.
The idea with double-sock mechanisms, including Armaskin socks, is that the lowest frictional interface is the sock-sock interface. The normal sock is the pink one here, the second sock is the yellow one. So the second sock stays in stationary contact with the skin. The normal socks stays in stationary contact with the shoe. And there is slippage between the two sock layers. This releases the skin to move in sync with the bone at an earlier moment in time, thereby reducing the magnitude of that shear deformation, with every step.
PRESSURE REDUCTION STRATEGIES
Basically, the harder two surfaces are pressed together, the higher the friction force. And the less hard they are pressed together, the lower the friction force, and the earlier we can get slippage at a material interface. This releases that area of skin so it can move in sync with the bone at an earlier moment. The effect will be at both interfaces – both the skin-sock and the sock-shoe interface.
I just want to elaborate on foot strike angle. Doug Richie and I were on the P3 podcast with Talysha a while ago and talking about my posterior heel blisters. Doug suggested that stride length could have been an issue, and this image, adapted from healthystep.co.uk, elaborates on why. As stride length and foot strike angle increases, the more posterior the ground reaction force is applied. So it moves more towards the posterior heel. Therefore, if you have a client that is over-striding and struggling with posterior heel blisters, this suggests that shortening their stride length may be a good idea. Particularly given that heel strike is likely when the largest shear event occurs at the posterior heel.
SHEAR ABSORPTION STRATEGIES
Shear absorption is a bit different because we’re not talking about relative motion at a material interface. We’re talking about the “give” in the material, or the shear deformation that happens within the material, external to the foot.
An example is a padded sock. I’ve got a double thickness pink line here for this padded sock. You’ll see the skin side of the sock remains in stationary contact with the skin, and the shoe side of the sock remains in stationary contact with the shoe. So there is no relative motion or rubbing between materials. But, as the calcaneus moves up, the skin is able to move up with it at an earlier moment because the sock itself undergo shear deformation. And then the same in the downwards direction.
Another example is a gel material applied to the skin. So the skin and the gel remain in stationary contact, and the gel and the sock remain in stationary contact. To reiterate, there is no rubbing between surfaces; all that’s happening is there is shear deformation occurring within the gel. This allows the skin to move in sync with the bone at an earlier moment in time, thereby reducing the magnitude of that shear deformation imparted to the soft tissues of the foot, with every step.
Gels can also be applied to the shoe, like Silipos sheeting. PelliTec pads are another example of something that attaches to the shoe and absorbs shear. Again, these materials undergo shear themselves. So, the pad is stuck to the lining of the shoe; and it remains in stationary contact with the sock. So there’s no relative movement anywhere, but there is deformation within the pad that allows the skin to move in sync with the bone.
SPREADING SHEAR LOAD
Shear load spreading is a bit harder to explain with these pictures I’ve been using. The easiest way I can describe it is to compare it to how cushioning works with the perpendicular load. So if this is a metatarsal head and there’s no cushioning, the perpendicular load is spread over a certain area and peak pressure is a certain amount. Now, if we implement some cushioning (eg: Spenco insole), then we’re spreading the same normal force over a larger surface area, thereby reducing peak pressure.
And so, it’s possible that if we’ve got peak shear at an at-risk location (eg: bony prominence), if we apply tape to this whole area, instead of that very discrete area of skin shearing back and forth and shear deformation being very pinpoint, we’re applying shear to a much larger surface area. We’re not getting rid of shear; shear is still happening in that skin, but we are potentially reducing peak shear at this particular location.
BONE MOVEMENT
Obviously if the calcaneus doesn’t have to move up or down in the sagittal plane as far, then shear deformation magnitudes will be lower. This is why potentially, calf stretches and things like heel lifts and heel height differential may be relevant. I can’t say that I’ve noticed a correlation between people that have big trouble with posterior heel blisters and people that are tight in the calf muscles, but you can see the theory here.
OTHER FACTORS
And to finish off, another couple of factors that we should consider include:
- Haglund’s deformity – because there’s more pressure.
- Frontal plane motion of the calcaneus – perhaps this may be relevant. I can’t say I’ve noticed a correlation.
- Unidirectional or bidirectional shear events – And finally the question of whether it’s a biphasic shear event or unidirectional shear event for the soft tissue at the posterior calcaneus. If we are having shear twice per step as opposed to once per step, then that’s double the shear. The more repetitive shear deformation is, the more likely it is that there will be that intra-epidermal fatigue that is the initiation of the blister injury.
Yavuz and colleagues in 2008 showed the byphasic shear episodes that occur on the plantar surface of the foot. The plantar forefoot experiences this bidirectional shear (both anterior and posterior). Whereas the planter heel only experiences the anterior shear event (unidirectional). This may possibly go some way to explaining why plantar forefoot blisters and ulcers are more common than plantar heel blisters and ulcers.
Recap
Okay, let’s wrap things up with the recap. I just wanted to give you a few nuggets to take away and chew on.
- Blisters are caused by repetitive shear deformation, not rubbing.
- Rubbing is not required for shear, or blister formation.
- Low friction rubbing reduces shear magnitude because it frees the skin surface so it can move in sync with the bone at an earlier moment, with every step.
- High friction rubbing sees higher shear magnitude plus risk of abrasion:
- Abrasion of the skin
- Abrasion of sock
- Abrasion of the shoe lining (I’m sure you have clients who wear holes in the back of their shoes)
- Shear is normal. The skin can put up with a lot of it. But that’s not to say it can’t become excessive in either magnitude or frequency (repetition).
- Shear isn’t visible. At least, it’s not easily visually appreciated, because it’s happening under the skin, within the foot.
- Rubbing isn‘t friction. Friction is the force that resists relative motion; rubbing is the relative motion. When we talk about blisters, we should not use the term “friction” to mean rubbing. They are not the same thing, they are far more opposite than similar.
- Rubbing can happen at any material interface:
- Skin-sock
- Sock-shoe
- Sock-sock
- COF reduction preventions promote earlier slip via reduced friction force.
- So do pressure reduction preventions, because F = COF x N
- Allowing rubbing doesn‘t mean the heel has to come out of the shoe – use lacing and all elements of optimised shoe fit to keep the heel in the shoe. But also recognise that it may be quite normal for the heel to move around 1.5cm relative to the shoe.
- And finally, we can reduce shear magnitudes by:
- Absorb it
- Spread it
- Reduce bone movement
- Reduce friction force
- Reduce COF
- Reduce pressure
Questions
Q1: Is the management of blisters the same in diabetics as it is in non-diabetic patients?
There are definite similarities in that the mechanism of injury of friction blisters is repetitive shear deformation, whether you’re diabetic or not. If we talk about ulcers, of course ulcers can be caused by other things like skin tears or scratches in the garden. They can also form after burn blisters, which obviously have a different mechanism of skin injury.
However, there are definite differences:
- Diabetics may have neuropathic and arterial insufficiency components that contribute to their friction blister injury.
- For example, pain perception can be reduced, so you can’t really expect and neuropathic diabetic to be able to nuance, fine-tune and troubleshoot blister areas, because they just won’t get the hotspot sensation.
- Perspiration is not an issue in diabetics with autonomic neuropathy. So that’s generally more of a non-diabetic aspect to blister formation.
- Soft tissue stiffness – The connective tissues in diabetics can be stiffer. This basically means it takes a lower magnitude of shear deformation to become injurious.
Q2/3: What are the best treatments / how to manage blisters
In terms of first aid, I encourage people to make the decision based on the integrity of the blister roof:
- If the blister roof is intact, we need to give a bit of protection to that skin, because it has lost its structural support from underneath, owing to the mechanical fatigue. So just an island dressing like a Band-Aid is really all we need (in terms of first aid).
- If the roof is torn, we need antiseptic to prevent infection, plus the island dressing. That island dressing will protect the damaged skin, and absorb fluids from the blister.
- If it is deroofed, we need the antiseptic to prevent infection, plus either an island dressing, or a hydrocolloid may be a better option. Why a hydrocolloid for this one? Because the hydrocolloid needs a raw wound base to be able to create the optimal conditions for healing, and that’s exactly what a deroofed blister is.
But of course, this is just first aid. If you want to implement the kind of treatment that is meaningful in terms of allowing someone to put their shoe back on and keep walking or running, in spite of that blister, then you have to implement something that is going to reduce the shear magnitude in the soft tissues. Without doing that, the blister will get worse. A Band-Aid or hydrocolloid alone is just not going to cut it. You have to have the blister prevention in place during blister treatment for it to be effective – to make the blister not painful, and to get some sort of momentum in terms of blister healing, in spite of the ongoing activity.
Q4: Strategies to prevent blisters for clients with fragile skin?
I had to think about potential reasons for fragile skin. Perhaps this means:
- This an elderly patient and they have fragile skin
- They have dermatitis or eczema or similar
- There a skin graft involved or scarring or healing ulcer
For any of these reasons, given we’re dealing with fragile skin, I’d be inclined to go top shelf right from the start, rather than trial less effective, but maybe easier to implement or easier to access strategies. So if we’re talking about posterior heel blisters for me, that’s Engo patches. That single intervention, in my experience, is all that needs to be done, as long as they are wearing a sock.
I probably wouldn’t want to adhere anything adhesive on fragile skin. So that takes adhesive products like tape, moleskin and felt donut pads out of the equation.
I probably don’t want to put anything topical on the skin either, like a lubricant. Another reason not to use a lubricant is that I wouldn’t want to encourage rubbing between the skin and the sock. We know that lubricant disperses into the sock and disperse away from where they are applied. As it does so, the effect is reduced such that friction levels increase above baseline. Our best guess as to how long that takes is an hour and a half. So after that time, friction levels to actually increase above baseline and therefore that rubbing may become abrasive, and obviously we don’t want that on fragile skin.
So in answer to the question, for posterior heel blisters, I would go straight for Engo patches. If you didn’t want to use Engo patches for some reason, I’d go with PelliTec pads next. They can be a good option at this list location. Otherwise, gels like Silipos gel sheeting work really well to absorb shear. However, I’m always a bit cautious about using gels when the is skin that’s already blistered or weepy for any reason, because the gel material doesn’t absorb fluids so it can accelerate maceration. I love using gel materials for lots of toe blisters as a prevention. But I don’t like using them on the toes as a part of treatment.
Next month
We’re going to talk next month about that research from Hashmi and colleagues in greater detail.
Got questions?
Hop over to our Pro site: pro.blister-prevention.com. This is purpose built for podiatrists and healthcare professionals. Look for the learn tab and select “Office Hours”. This is where we have our replays. And if you have a question, you can pop it in the comments section – I’ll get an alert and I’ll be straight on there to answer your question.
Thanks for joining me again, and we’ll see you on the first Wednesday of March for our next episode of Blister Prevention Office Hours.


2 Responses
What is the volume of perspiration per foot per day on average?
i read somewhere, sometime 300mls?
Hi Joanne 🙂
Sweat production in the foot has been estimated to range between 381 to 447 grams per hour.
– Taylor NAS, Caldwell JN, Mekjavic IB. The sweating foot: Local differences in sweat secretion during exercise-induced hyperthermia. In: Aviation Space and Environmental Medicine. Vol 77. 2006.
– Fogarty A, Bartlett R, Ventenat V, Havenith G. Regional foot sweat rates during a 65 minute uphill walk with a backpack. In: Mekjavic I, Kounalakis S, Taylor N, eds. Environmental Ergonomics XII. Proceedings of the 12th International Conference on Environmental Ergonomics. 2007:283-284.