Thank you for joining me on this episode of Blister Prevention Office Hours. We’re going to be looking at the Hashmi et al (2013) study today, all about posterior heel blisters. I had intended to look at this in greater detail last month, but it just morphed into its own presentation. So now we’re going to be talking about this paper. If you didn’t catch last month’s episode, I highly recommend you take a look because it was a really good discussion about posterior heel blisters and all the relevant factors. We had a good look at the relative motion scenarios at heel lift and heel strike; had a quick look at research; and we delved into quite some depth on how the prevention’s work. So if you are here to look at what works as a blister prevention for the posterior heel, then definitely head back to last month’s episode and watch that.
What we’ll cover
So yeah, we’re going to look at the Hashmi research. We’ll look at the aims, the methods and all of the findings and implications. This paper is titled: The formation of friction blisters on the foot: the development of a laboratory-based blister creation model, and it was in Skin Research and Technology. It was by Farina Hashmi, Barry Richards, Saeed Forghany and Chris Nester. What they did was they produced blisters on the posterior heel with this jig; I’m going to explain this in more detail in a moment.
Aims
So the aims were twofold. What they wanted to do was have a look at how digital infrared thermographic imaging correlated with the contact method of temperature measurement, which was just a normal thermometer basically where it’s actually touching the skin to get the measurement. And also to describe the temperature changes before, during and after blister formation.
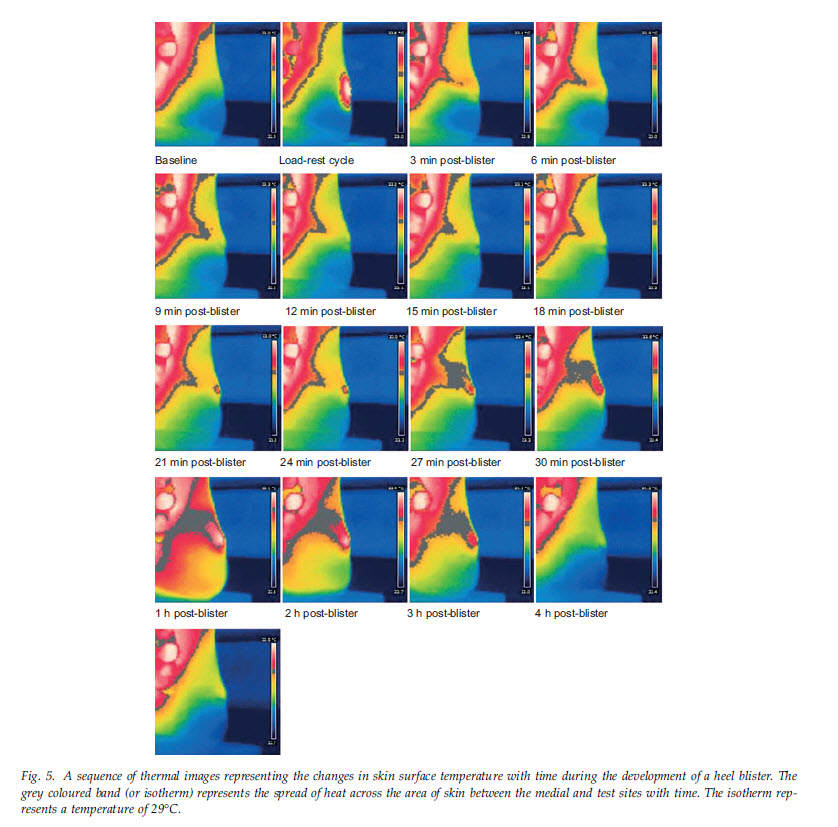
This is what a digital infrared thermographic imaging camera looks like. I got this picture off eBay – you can buy this for $200AUD. This isn’t the exact model they used but it would have been this kind of camera which produces this kind of image. And this is an example of the images that they were able to produce, before, during and after blister formation indicating temperatures and temperature change.

Methods
There were 30 subjects and they had this load application mechanism (LAM) set up which looks fantastic. It’s a spring operated rotating load applicator with a curved surface covered with textured rubber providing a high frictional interface with the skin. So basically as that applicator moved up and down, because of the high friction level, it would grab the skin so the skin moved with it, thereby creating the shear deformation in the soft tissues between skin surface and bone. And temperature readings were taken before, during and after blister creation.
How much did this load applicator move? It moved 15mm (1.5cm). It seems like a lot. But the reason they used that amount was they found in an unpublished pilot study that that’s how much the foot moves relative to the shoe at heel strike. Being unpublished, we couldn’t take a bit of a look at it in more detail, but I think this needs verification. I’m not doubting that it’s true. But I have a feeling that most podiatrists wouldn’t be comfortable with the fact that the heel moves relative to the shoe 1.5cm with each step. Presumably there’s a bit of heel fat pad compression that’s responsible for that. But how much is the foot moving up relative to the shoe at heel lift? Because presumably what goes up must come down. So that would be a tidy little experiment for someone who’s got some slow motion high speed video to actually replicate and publish.
The loading cycle: So the load applicator was operated at a rate of 120 passes per minute. So it went up and down for two minutes and that speed was chosen to replicate fast walking. And so the load was applied for two minutes and then there was a one minute break so they could take the temperature recordings, and also to inspect the skin to see whether a blister had formed, because that was the endpoint of the load application.
Temperatures were recorded every three minutes during the load/rest cycles until blister formation. And every three minutes for the 30 minutes post blister formation. The subjects remained standing and had those measurements taken every three minutes. And then for the next five hours, the temperature was measured every hour, and the participants were allowed to leave the room at this stage. They just weren’t able to wear shoes on any of these areas of their foot.
Endpoint: As I mentioned, the endpoint of the loading was the initiation of the blister injury and that was determined by skin inspection. They were looking for a blanched area of skin within an erythematous inflamed area of skin, and a visible pleat of epidermis lifted from the underlying dermis. So that’s what it looks like when a blister first forms and hasn’t yet had a chance to fill with fluid.
Findings and implications
So let’s get to the meat of this discussion. We’re going to talk about the researchers findings and the implications of this research.
Clinical signs: First of all, there was a consistent pattern of clinical signs that was redness initially. They termed this a hot spot. It’s probably not that important, but is a hotspot a clinical sign or is it a subjective symptom? I think a lot of people (our patients) use the term hotspot as a symptom rather than something that they see. But as I said, it’s not important to this discussion. So these clinical signs were initial redness, blanching of the skin in response to load, and the appearance of a small pleat of epidermis that subsequently filled with fluid. It takes up to two hours to fill with fluid, but is usually filled in around an hour; iIt’s not full of fluid straight away.
Symptoms: A consistent pattern of symptoms were described. That is, an initial rubbing sensation, followed by a stinging sensation, which then subsided until a sharp pain felt, heralding the initiation of a blister. This is in line with other descriptions surrounding blister formation.
Time to blister: Time to blister varied greatly in this study. It was between four and 32 minutes. The authors speculated this variation could be due to surface hydration. Definitely, different people will sweat at different rates over that time. But it could just be the intrinsic resilience to shear strain over that time. Everyone’s skin and subcutaneous tissue can deal with repetitive shear load a bit better or less so than others. And if we look at the other experimental blister research papers, we can see that there is this vast range of time to blister. Sulzberger et al, who produced blisters on the palms, found it took from three minutes to over 50 minutes of loading. Some people still hadn’t blistered after 50 minutes. And Naylor, who produced blisters on the anterior shins back in 1955 found it took between 27 and 138 load applications for blistering to occur. So there’s a big difference between subjects.
Temperature recordings: Remembering that the researchers were looking to see if there is a correlation between the contact and the non-contact forms of temperature measurement; they found that there was good correlation. The degrees Celsius wasn’t exactly the same but the changes all correlated very well. So the good thing about this is it supports the use of a non-contact way of measuring temperature which obviously has advantages because when you apply a thermometer to the skin that could cause a change in skin temperature. Plus there’s the need for contact, so there is time involved. So yeah, the non-contact method has many advantages.
Temperature change: Temperatures increased from baseline to blister formation. Then, once the blister formed and the load was no longer applied, temperature reduced. Looking at that in a bit more detail.
Baseline to blister formation:
- At the control site, temperature remained relatively constant
- At the test site, the median temperature increase was 5.1 degrees Celsius (range was 1.7 – 9.9 degrees Celsius).
Of note, in future papers that used a similar setup to this, they used a temperature increase of three degrees Celsius as indicative of imminent blister formation. But three degrees wasn’t mentioned in this paper. So they’ve obviously done further statistical analysis to come up with that three degrees.
Thirty minutes after blister formation, temperature had reduced significantly, but it was still above baseline. And it was still above baseline albeit significantly reduced five and a half hours after the load had finished. So that’s a long time, and still temperatures were above baseline, very slightly.
Implications of temperature change: The authors discussed, since the skin temperature increase after repeated applications of load, it is reasonable to assume that a physiological inflammatory response was initiated and responsible for the recorded skin temperature increases. This demonstrates that our method quantified the pre- and post- blister physiological inflammatory changes that occur in response to external loads. Also that these temperature changes were not due to superficial frictional heat, nor changes in environmental temperature, at least for up to 30 minutes post blister – remember after that time they were allowed to leave the room and so the ambient temperature wasn’t standardized.
Unexpected temperature finding: The concurrent rise in the temperature of the skin site between the medial malleolus and the back of the heel was not expected. This was noted in all participants, but presented at different times during the experiment and the surface areas affected by this heat varied. So, that’s shown on each of these images. There’s a big red patch at the top left and then you can see the blister at the back of the heel which is a bit to the right of that. And you can see this spike of temperature between the two. So, that was something they didn’t expect to see. The authors mention: This phenomenon might offer a surrogate measure of events occurring at the site of the blister. This has the added value of providing us with a site that can be used for data collection whilst the test site is physically covered for example by footwear or a blister dressing. So, potentially if we could measure temperature change somewhere other than the blister site, we could cover that blister site with a blister prevention, and test how effective it was at reducing temperature change while load was applied. This really is fascinating!
Skin thickness: It was anticipated that the subcutaneous tissue thickness would not vary greatly at this site and it was not measured. However, observations made by palpation and during load applications showed that the tissue thickness at the test site did vary between participants. So this is quite fascinating, too. If you think about tissue thickness, it might help to compare the thin skin on the back of your hand (or dorsum of the foot) to the thick skin on the palm of the hand (or plantar surface). The epidermis is 9% thicker on the plantar surface than it is on the dorsal surface of the foot. Plantar and palmar skin is thick and well-tethered to underlying structures. Whereas dorsal skin of the foot and hand are thin and loosely tethered.
The authors say this corroborates the work conducted by Sulzberger, but go on to contradict themselves. I’m not sure whether they got themselves mixed up with this, or whether I’m reading it wrong, or whether they actually found different things to Sulzberger.
To clarify, this is what Sulzberger found in terms of blister formation. Basically, we need a thick epidermis to be able to withstand repetitive shear deformation to be able to remain intact and hold a fluid-filled lesion; and it needs to be adhered firmly to underlying structures. Essentially, they say these prerequisites explain why friction blisters do not generally occur where the skin is loose or the stratum corneum thin. That is why palmar and plantar skin, and such sites as the heels (I presume they’re talking about the posterior heel) blister most regularly in response to friction. They have both of the necessary requirements: a thick stratum corneum for the blister roof; and tight adherence of the skin to underlying structures.
For clarity, what happens when we produce blisters on thin skin is, at the point of the intra-epidermal tear (ie: the initiation of the blister injury), the roof rubs off straight away, because it’s just not able to withstand the repetitive shear deformation that continues to occur. That’s why we get more fluid-filled blisters on thick skin. When we get blisters on thinner skin, they tend to deroof because it just can’t sustain or withstand repetitive sheet information.
But I do agree with Hashmi and colleagues when they say future work in this area should consider the use of ultrasound imaging to clarify the possible contribution of the subcutaneous tissue mechanics to skin blistering. I would just be fascinated to understand that in more detail.
Compressive force: Although the degree of compression applied by the load applicator was standardized (70kPa), it is not clear how this level compares with actual forces experienced by the skin at the posterior heel when walking in a shoe. What is normal peak pressure at the posterior heel? Has it ever been measured? I don’t know. I couldn’t find any information.
Unidirectional or biphasic?: We spoke very briefly about this last month. Is the shear event at the posterior here, unidirectional, or biphasic? This experiment created a biphasic shear event; a shear event up and a shear event down. But then the authors discuss how it’s actually the shear event that happens at heel strike, which is the most important. And perhaps they should have just produced a shear event that mimicked heel strike. They say the heel strike shear event is more important, but they don’t actually provide a reference. So I think there’s a little bit of work to be done here. Is the shear event that happens at heel lift negligible? Or is it something that should be considered.
The reason it’s important is, blisters are caused by repetitive shear deformation, and the repetitive part of that is important. If shear is happening twice per step rather than once per step, then blisters are going to occur more readily. Yavuz 2008 showed the shear events on the plantar surface. They showed how the plantar forefoot undergoes a biphasic shear event with every step. Whereas the plantar heel only has one shear event per step. This may go some way towards explaining why plantar forefoot blisters (and ulcers) are much more common than plantar heel blisters (and ulcers).
Concluding statements
Just to really hammer home how important this research was and how fascinating it was, here are a few quotes and paraphrases from this research.
“The factors causing the formation of foot blisters cannot be precisely controlled or really analyzed in field conditions.” So this little set up really was fantastic.
“This paper describes how change in skin temperature can be quantified non-invasively during the formation of friction heel blisters. This is the first report concerning the controlled creation of foot blisters and the concurrent measurement of physiological change within the skin.” Definitely!
“The load application mechanism was able to provide the appropriate amount of compression and friction forces to the skin to generate friction blisters.” So yeah, it was a really great little piece of kit.
“The scale of temperature change during these stages of blister creation, along with the consistency across subjects, suggest that temperature would be a suitable measure for testing risk factors associated with friction blister formation.”
“Moreover this information will contribute to a greater understanding of how prevention or treatment strategies might interfere with the underlying risks of blister formation.” So, we can implement prevention, apply load, and measure temperature change and compare it to temperature change without the intervention. This could show some very interesting information about how effective a prevention is.
“Creating blisters on the feet for the purposes of research does expose participants to risk. The need to cause blistering in future may not be necessary as these data clearly show measurable changes in temperature in the time preceeding blister creation.” And this was indeed used in a couple of papers subsequent to this one. These subsequent papers used a temperature increase of three degree to indicate imminent blister formation. Again, I don’t know where the three degrees comes from because it wasn’t a conclusion or discussed finding of this 2013 paper. I can only assume they performed additional statistical analysis on the data from this paper.
The first of these subsequent papers was in 2014 by Suzanne Kirkham, Sharon Lamb, Chris Nester and Farina Hashmi looked at skin hydration. They basically put one foot in a bucket of water, and one remained dry, and they applied the shear load. It looks like an updated version of the original LAM. They found that the hydrated skin had an increase in temperature much faster than the dry skin.
Then, in 2016, they tested three prevention strategies. So paper was authored by Farina Hashmi, Suzanne Kirkham, Chris Nester and Sharon Lamb. They looked at 2Toms Blistershield powder, Flexitol Blistop, and Boots antiperspirant. They found that there was no significant difference in temperature changes with and without the intervention. So that was interesting. This suggests these preventions don’t work. It would be great to be able to just apply this to all the preventions in the world and see whether we can find something that does affect temperature change. To my knowledge, these are the only follow up studies that have been done.
So yeah, fantastic work by Farina Hashmi and colleagues; really enlightening! I wish I had that jig to be able to have a bit of a play with and even the infrared camera.
Q & A
That concludes this discussion, so now we’ll move on to the Q&A. If you’ve got a question and you’re on the call, just feel free to either put on your microphone or type it in the chat.
We got three questions at the time sign up – thank you for the questions that came in. They’re all kind of along a similar theme: sweaty feet; and are moisture levels important to the formation of blisters; and moisture-wicking socks.
What do I want to say about moisture… Is important to the formation of blisters? Yes, it’s one reason why there is increasing friction force at the skin, which increased the risk of friction blister development. Is it the be all and end all of blister prevention? Definitely not. It’s important to manage moisture to some degree. But it’s not the only way to prevent blisters. We can prevent blisters in more sophisticated ways and allow foot skin to be damp. There’s nothing more frustrating to me when people contact me and indicate that they’ve kind of given into the inevitability of blisters because they recognize the fact that they can’t keep their feet dry. So basically, yes, let’s manage moisture. If you’d like to listen to a good discussion on all the ins and outs of this, I did a presentation about a year and a bit ago on the moisture management strategies. We look at powders, antiperspirants moisture-wicking socks and more. I won’t go through all that now as we don’t have the time. But definitely head over to pro.blister-prevention.com/office-hours and listen to that.
Maryann asked “is moisture wicking material socks better than Merino wool.” I did a presentation on this little while ago too. Check that one out because it goes through everything in more detail. I wish I had an easy quick yes or no answer. But the fact is, we don’t know. Doug and I have spoken about this a lot. Doug is quite the authority on socks and blister management. I’m going to put a link to our paper in the chat, because it lays out all the research to date on this topic.
My advice is get a sock that’s comfortable. Thicker is better than thin in theory, but that’s not to say that if you wear thin socks, you’re going to get blisters. If it’s cold, wool is probably the better choice thanks to its thermal insulation.
Wrapping up
Okay, guys, I think that that is about any questions. If you ever want to watch a replay, they are all posted on our pro site at pro.blister-prevention.com/office-hours. Click on the Learn tab here and you’ll find office hours. That’s where we keep the replays.
If you have any questions, send me an email. We’ll be here the first Wednesday of every month. If there’s a topic that you want me to cover, let me know and I’ll definitely consider it. At the moment, I don’t know what I’m discussing next month.
Hope you learned a little bit from today’s presentation. Thanks to Hashmi and colleagues for this brilliant study. So with that, I will say goodbye and thanks for joining me and we shall catch you later. Bye for now.